Acknowledgments
All Survivors Project (ASP) and Youth Health and Development Organization (YHDO) would like to thank the victims/survivors of sexual violence, healthcare providers, community health workers and government and non-government stakeholders who participated in this research and shared their perceptions and experiences. The report was authored by Julienne Corboz. Layout and production assistance was provided by Roberto Thillet. ASP and YHDO, and the author of this report, are extremely grateful to the stakeholders who participated in the National Advisory Group, particularly those who peer reviewed and provided valuable feedback on drafts of the report, including: Taiba Jafari, Director of the Gender Directorate, Islamic Republic of Afghanistan Ministry of Public Health; Najeebullah Zadran Babrakzai, National Coordinator for the Rights of Children, Afghanistan Independent Human Rights Commission; and Palwasha Aabed, Child Protection Officer, United Nations Assistance Mission in Afghanistan. The author is also grateful for peer review and feedback from the ASP and YHDO team. All Survivors Project, and not the peer reviewers, is responsible for the final content of this report.
Cover illustration: Brian Stauffer
© 2021 All Survivors Project and Youth and Development Organization.
Acronyms
ASP – All Survivors Project
BHC – Basic Health Centre
BPHS – Basic Package of Health Services
CHC – Comprehensive Health Centre
CHW – Community Health Worker
CPAN – Child Protection Action Network
CRSV – Conflict-related sexual violence
DoPH – Department of Public Health
EPHS – Essential Package of Hospital Services
ER – Emergency room
EVAW – Elimination of violence against women
FLE – Family Life Education
FPC – Family Protection Centre
GBV – Gender-based violence
HIV – Human Immunodeficiency Virus
HSC – Health Sub-Centre
IDI – In-depth interview
KII – Key informant interview
MoE – Ministry of Education
MoLSA – Ministry of Labor and Social Affairs
MoPH – Ministry of Public Health
MSM – Men who have sex with men
NGO – Non-governmental Organisation
OPD – Outpatient department
SOGIESC – Sexual orientation, gender identity and/or expression, and sex characteristics
SOP – Standard operating procedure
STI – Sexually transmitted infection
UNFPA – UN Population Fund (previously UN Fund for Population Activities)
YHDO – Youth Health and Development Organization
WHO – World Health Organization
EXECUTIVE SUMMARY
Women and girls in Afghanistan are extremely vulnerable to gender-based violence (GBV) and face substantial barriers accessing healthcare facilities to seek help after such violence. This is widely known. Much less is known about sexual violence committed against men and boys, the barriers male victims/survivors face accessing healthcare facilities, or the quality of healthcare provision available to them.
This report presents the findings of research conducted by international non-governmental organisation All Survivors Project (ASP) with its partner on the ground in Afghanistan, Youth Health and Development Organization (YHDO). With this research, ASP and YHDO seek to:
- Cast light on the healthcare needs and experiences of male victims/survivors of sexual violence in Afghanistan and the barriers they face accessing quality healthcare services.
- Understand the practices of healthcare providers, and the barriers they face, in supporting male victims/survivors of sexual violence.
- Learn about how a survivor-centred approach to healthcare provision is applied in Afghanistan in the case of male victims/survivors.
- Produce a set of recommendations for enhanced survivor-centred healthcare services for male victims/ survivors of sexual violence that can be used to develop a tool for the health sector.
The research was conducted in three provinces of Afghanistan: Kabul, Balkh and Kandahar, with data collection conducted during the second half of 2020, under special measures adopted in light of the COVID-19 pandemic. The research adopted a qualitative approach involving four key methods:
- A desk review, including literature on sexual violence against men and boys and the health sector response, with a focus on evidence from Afghanistan.
- A stakeholder mapping to identify existing systems of healthcare response that include coverage of male victims/survivors, conducted predominantly through a desk review of online documents.
- Ten key stakeholder interviews were conducted with a range of individuals, from government, national and international NGOs, and UN agencies.
- Ninety-seven in-depth interviews were conducted – 27 with male victims/survivors of sexual violence, 44 with healthcare providers working in different types of static health care facilities, and 26 with community health workers.
The results of the ASP/YHDO study suggest that the health sector is currently a vastly underused entry point for male victims/survivors of sexual violence in Afghanistan, due to multiple and cumulative barriers preventing them from accessing healthcare services.
Before elaborating on these barriers, the report outlines the structure of Afghanistan’s healthcare system under which services operate at three main levels: community, district, and provincial/regional. There is an upward referral system under which more complex cases are referred to higher levels where there are larger numbers of healthcare staff, services and resources. In addition to the different types of static and mobile health services overseen by the Ministry of Public Health, some health facilities are run privately.
A range of services has been developed specifically to address the health care needs of victims/survivors of GBV, although these are largely directed towards women and girls. Thirty-seven Family Protection Centres (FPCs) have been established in 26 provinces and form part of a wider multi-sector response to GBV programme that provides health, police and justice services for victims/survivors, with FPCs providing the primary entry point. FPCs are located in government provincial and regional hospitals to ensure their sustainability within the national health system, and provide support to victims/survivors, including basic health services, medical support, psychosocial counselling, legal support, help in collecting evidence and providing referrals to other services. FPCs may not be accessible for all victims/survivors, particularly those who live in more remote locations. Consequently, some NGOs working in humanitarian response now send mobile outreach teams to visit communities and provide GBV services and referrals.
Several resources have been developed by a range of organisations to facilitate higher quality of health care provision for victims/survivors of GBV, although, much like GBV services, these resources are largely directed towards women and girls. These include a training manual for health professionals on a traumasensitive approach to care for victims/survivors of GBV in Afghanistan; Standard Operating Procedures for Healthcare Sector Response to GBV; and the GBV Treatment Protocol for Healthcare Providers in Afghanistan (GBV Treatment Protocol).
The GBV Treatment Protocol contains comprehensive information and guidance on a range of topics, including legal frameworks and requirements, patient flow, confidentiality, documentation and reporting, survivor-centred care, identifying and responding to patient disclosures of GBV, and different types of care for victims/survivors. The Protocol is intended to provide guidance on healthcare response to all GBV victims/ survivors; however, although it notes that men and boys, particularly adolescent boys, can experience sexual exploitation and violence, the Protocol emphasizes that women and girls are disproportionately affected by GBV and the Protocol is largely targeted towards them.
The barriers preventing male survivors/victims of sexual violence accessing quality healthcare services are detailed in the ASP/YHDO report and are outlined in Table 1 below. Adopting a social ecological model of public health, the barriers are differentiated by level, of which there are five: individual, interpersonal, community, organisational, and structural. These barriers do not operate in isolation and male victims/survivors face multiple, mutually reinforcing barriers, making access to healthcare services extremely challenging.
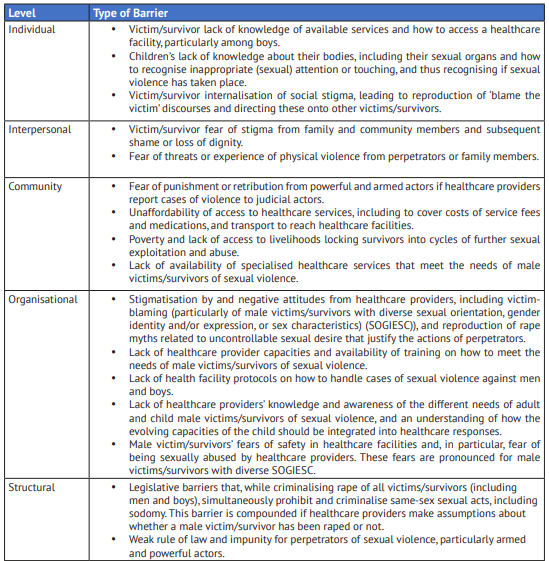
Poverty and inability to pay for services, including fees in private healthcare facilities (which are often perceived to be of higher quality and safer) and for medications or other services in government facilities, were highlighted as important barriers. Further, victims/survivors with poor socio-economic status living in rural or remote areas were reported to struggle to pay for transport to access a healthcare facility at the district level or in the provincial centre.
The legal and policy environment in Afghanistan in relation to male victims/survivors of sexual violence appears to be an important structural barrier to help-seeking. Despite no legal requirements for mandatory reporting of GBV cases in Afghanistan, male victims/survivors reported strong fears that healthcare providers would disclose their case to judicial actors without their consent. These fears are likely linked to same-sex sexual acts being criminalised and concerns that, despite rape being criminalised under the Penal Code, healthcare providers will make judgements about whether sexual acts are consensual or non-consensual. The research found some examples, specifically in Balkh province, where this appears to be the case.
The research identifies several rape myths that circulate about why sexual violence against men and boys occurs. Male victims/survivors are more likely to reproduce victim-blaming discourses, perhaps due to internalised stigma and blame received from others. In contrast, healthcare providers are more likely to justify the behaviour of perpetrators by suggesting that social and cultural norms and practices, including expensive weddings and gender segregation, lead to men’s uncontrollable sexual desire. In either case, perpetrators are not portrayed as being actively responsible for the sexual violence they perpetrate, with the locus of responsibility being placed on victims/survivors and their families.
The ASP/YHDO report examines how communities might support male victims/survivors of sexual violence. It suggests that community health workers (CHWs) could play a role in supporting male victims/survivors and facilitating their access to health facilities, although there are gaps in CHWs’ knowledge of how to provide confidential and survivor-centred care. The report also suggests that community leaders, religious leaders and members of community health councils may also have a role to play in reducing barriers to male victim/survivors’ access to healthcare facilities by raising awareness of and preventing stigma against male victims/survivors and supporting them to access services. However, significant work needs to be done with community and religious leaders to challenge their negative attitudes and potentially violent behaviours towards male victims/survivors.
The report describes the perspectives of male victims/survivors and of healthcare providers on the care pathway for male victims/survivors in health facilities, and the typical experiences that men and boys might expect to have in receiving care, including survivor-centred care. The majority of the healthcare providers interviewed had knowledge about the characteristics of a survivor-centred approach and in most cases were able to articulate how such an approach would be implemented with male victims/survivors, even though few of them had ever provided services to a male victim/survivor of sexual violence.
The descriptions given by healthcare providers on how to implement such an approach were largely in line with the guidance provided in the GBV Treatment Protocol, despite few of them having been trained in the use of the Protocol and the Protocol being largely framed around the needs of women and girls. To identify and illustrate the extent to which current practices and systems to address the needs of male victims/ survivors are aligned with the GBV Treatment Protocol, the ASP/YHDO research findings are set alongside the guidance in the Protocol – including its guidance to ensure respect, empathy, and non-judgement, to ensure privacy and confidentiality, and in relation to the question of referrals to judicial actors, and of survivor choice and control.
Despite the healthcare providers’ overall knowledge of survivor-centred care, the report points to significant dissonance between their descriptions of the care they would provide to a male victim/survivor, and the treatment that male victims/survivors expect to receive. This could be due to victims/survivors being unaware of more recent advancements in health sector responses to GBV more generally. However, it may also be due to persisting gaps in healthcare providers’ attitudes, knowledge and practices with regards to male victims/ survivors of sexual violence.
For ethical and safety reasons, the victims/survivors interviewed for this research were all adults, leaving an acknowledged gap in the research. However, several male victims/survivors disclosed that they had first experienced sexual violence as a child. Healthcare providers also described how services may differ for boys in comparison with adult men, and several healthcare providers reported having previously provided services to boy victims/survivors of sexual violence. Consequently, some retrospective analysis of healthcare provision for boys is provided.
Healthcare providers did articulate barriers that boy victims/survivors of violence face in accessing healthcare services, including lack of knowledge of how to access a facility. However, healthcare providers appeared to lack awareness of the different needs of adults and children, and an understanding of how the evolving capacities of the child should be integrated into healthcare response. This may be due to most of the healthcare providers interviewed never having provided services to male victims/survivors of sexual violence, whether boys or adults. However, lack of understanding of or capacity to implement an approach that recognises the evolving capacities of the child was also found among healthcare providers who reported having provided services to girl victims/survivors of sexual violence, suggesting that there is a wider gap in this area.
More broadly, the research identifies other gaps in the provision of healthcare services to male victims/ survivors of sexual violence. Healthcare providers emphasized, for example, the unavailability of psychosocial services for victims/survivors of violence, and the lack of capacity of psychosocial counsellors to deliver services specifically to male victims/survivors of sexual violence.
One of the most important healthcare needs of male victims/survivors of sexual violence is to be treated with no judgement, blame or stigma. Victims/survivors also strongly emphasised the importance of confidentiality and the need to trust that a healthcare provider would not disclose their case to family or community members and, importantly, judicial actors, without their consent. Healthcare providers also emphasised the importance of these principles of care; however, it is unclear the extent to which they are implemented in practice. The research findings suggest that some healthcare providers may reproduce blame or stigma when male victims/survivors of sexual violence engage in sex work or if they identify as having diverse SOGIESC.
Further, the research points towards a possible gap in healthcare providers’ recognition of male victims/ survivors with diverse SOGIESC as a vulnerable group in need of services, or as legitimate victims/survivors of sexual violence. This lack of recognition may be due to assumptions that male victims/survivors with diverse SOGIESC who access health facilities for sexual violence have in fact consented to sexual acts and, thus, that these cases should be classed as sodomy, which is illegal under the Afghan Penal Code. It is unclear from the research what kinds of legal provisions healthcare providers are required to abide by with regards to male victims/survivors of sexual violence, including respect for confidentiality and rights to instigate the criminal justice process or not. Although the GBV Treatment Protocol articulates legal provisions for female survivors, the protocol does not articulate the rights of male victims/survivors of sexual violence.
Concerns about stigma and shame feed into victim/survivors’ fears of disclosure of sexual violence to healthcare providers, and subsequent fears that they may be punished or experience further violence from perpetrators or even families if healthcare providers breach confidentiality and share their cases with others, including judicial actors. Victims/survivors also reported fears of being raped or sexually abused by healthcare providers and suggested that male victims/survivors with diverse SOGIESC may be at particular risk. These fears of confidentiality breaches, or of experiencing further sexual violence at the hands of a healthcare provider, feed into deep lack of trust in healthcare provision, which restricts victims/survivors from accessing a healthcare facility or disclosing their experience of sexual violence to a healthcare provider.
RECOMMENDATIONS
In light of the research findings, ASP and YHDO make the following recommendations based on the various levels and types of barriers that male victims/survivors face in accessing quality healthcare services. Although many of these recommendations are targeted towards the health sector, enhanced male victim/survivor access to healthcare services requires a multi-sectoral approach, and the recommendations reflect this need.
Recommendations to the Government of Afghanistan
Ministry of Public Health (MoPH)
- Raise awareness of the availability of healthcare services for male victims/survivors of sexual violence, including the types of healthcare facilities available that can meet their needs, and the protocols in place to protect their rights (e.g., confidentiality protocols, and mandatory reporting not being legally required). This can be done through targeted media campaigns, drawing on social media, television, radio and print media, and can also expand existing media disseminated by the MoPH, NGOs and civil society on healthcare provision to GBV victims/survivors.
- This recommendation is contingent on a greater understanding of the extent to which both government and non-government run healthcare facilities have the necessary protocols and services in place for male victims/survivors; to this end, a comprehensive mapping should be conducted.
- Develop specialised services for male victims/survivors of sexual violence, including boys, within public health facilities.
- This could involve expanding existing services targeted towards women and girls, such as Family Protection Centres (FPCs), and increasing the human resource and technical capacity of healthcare providers in these facilities to provide services to men and boys, including specialized social workers and counsellors, particularly for boys.
- Specialised services could also involve opening sections of regional and provincial hospitals that are resourced to provide services to male victims/survivors of sexual violence.
- Men and boys, particularly the latter, may be uncomfortable sharing their experiences with male healthcare providers given their experiences of abuse. Consequently, any specialised services should include both female and male healthcare providers and focal points and men and boys should be given the choice of the gender of the healthcare provider they consult with.
- Male survivors may fear for their own safety within a healthcare facility, including being emotionally mistreated, or experiencing inappropriate touching or unwanted sexual advances. Healthcare facilities should implement safeguarding policies that allow all victims/survivors to report any breaches of safety, with corresponding systems for independent follow up to and investigation of reports, and guarantees that victims/survivors will not be punished for reporting safety breaches. Victims/survivors should be made aware of safeguarding policies when accessing a healthcare facility and staff should be briefed and oriented on safeguarding policies and made aware of the repercussions if they do not comply.
- Conduct specialised training with healthcare providers on knowledge, attitudes and healthcare practices related to male victims/survivors of sexual violence.
- Ensure that the training challenges identified myths about the causes of sexual violence against men and boys and justifications for the actions of perpetrators. Healthcare provider misconceptions about the drivers of conflict-related sexual violence (CRSV), and that armed perpetrators rape men and boys due to lack of education rather than weak rule of law and subsequent impunity, should also be addressed in training.
- Ensure that the training addresses how to enhance victim/survivor feelings of safety, including: treating the survivor with respect and empathy and not using any humiliating language; always asking for the consent of the survivor before physical examination, including of parts of the body associated with the sexual violence, and explaining at all times what the physical examination entails and how it will be performed; and giving the survivor the choice of having another person present during the medical consultation.
- Ensure that the training addresses healthcare provider capacity gaps identified in the research, including providing survivor-centred care to male victims/survivors at high risk of violence, such as those who engage in sex work or those with diverse SOGIESC.
- Ensure that the training addresses the evolving capacities of the child and how to integrate knowledge of these capacities into provision of care for child victims/survivors of sexual violence, including boys.
- Train and support CHWs to implement survivor-centred care when providing support to victims/survivors and referring them or facilitating their access to static healthcare services.
Ministry of Labor and Social Affairs (MoLSA)
- Develop and implement reunification and reintegration programmes to facilitate male victims/ survivors to return safely to their families and communities.
- Strengthen the provision of livelihood support for male victims/survivors of sexual violence, both to ensure they have sufficient economic capital to access quality healthcare services, and to assist them to exit situations of sexual exploitation and abuse and to draw from alternative livelihoods options.
- Although healthcare providers and the MoPH are not well placed to support victim/survivors’ enhanced livelihoods, advocacy with other government bodies, particularly the MoLSA and NGOs supporting livelihoods of GBV victims/survivors, should be conducted and livelihoods support should be expanded to include male victims/survivors.
- Livelihoods programmes for male victims/survivors could involve family-level activities, both to enhance livelihoods at the household level and support efforts for reunification and reintegration of victims/survivors into their families and communities (see recommendation six).
Ministry of Education (MoE)
- Children’s lack of knowledge about their bodies, including their sexual organs and how to recognise inappropriate (sexual) attention or touching is an individual barrier, but one that requires interventions at the structural and community levels.
- Raise children’s (both boys and girls) knowledge and awareness of the risks of sexual violence by providing age-, culturally- and Islamic-appropriate Family Life Education (FLE). Although efforts to do this are underway, further advocacy is needed with the MoE to ensure that FLE materials are included in the national curriculum.
- Raise awareness in communities and families about the importance and acceptability of FLE, for example through targeted media campaigns and dissemination of information through community events, including through mosques.
Ministry of Justice
- Stronger measures must be put in place to ensure rule of law and accountability for all forms of sexual violence against men and boys, including CRSV. The revised Penal Code, including provisions relating to the banning of bacha bazi and all forms of child exploitation and abuse, should be widely disseminated in accessible formats. Recipients must include all national and local government officials, members of the judiciary and the Attorney General’s Office, the state security forces, community and religious leaders, teachers and others in positions of authority or influence. An effective and comprehensive victim and witness programme must be set up to enable survivors of sexual violence to safely report their case and pursue justice.
Recommendations to National Organisations
Health Sector NGOs
- Given that stigmatisation by family and community members, and subsequent threats of violence and abuse, are strong barriers to male victims/survivors accessing healthcare services, awareness-raising activities should be implemented at the community level.
- Train and support community level actors, including CHWs, community and religious leaders, and members of community health councils, to raise awareness of sexual violence against men and boys, reduce stigma against victims/survivors and support them to access healthcare services. Awareness raising, training and support must involve content on the importance of treating victims/survivors as victims rather than offenders.
- Given that male victims/survivors of sexual violence may be internalising victim-blaming discourses, work closely with them to reduce self-blame for the sexual violence they have experienced, and raise awareness of, and challenge, internalised stigma directed onto other male victims/survivors.
- Psychosocial counsellors are important actors in supporting this process of reducing self-blame and challenging the internalisation of stigma, and their capacity should be built to facilitate this process.
Recommendations to International Multi-Lateral Agencies
World Health Organization
- Update the GBV Treatment Protocol, or include an annex, with specific content on the needs of male victims/survivors of sexual violence, including boys and adult men and those with diverse SOGIESC. The updated protocol should aim to fill gaps in healthcare provider knowledge, attitudes and practices identified in this report, including those articulated in recommendation four.
- Ensure that the updated GBV Treatment Protocol or annex clearly articulates the legal rights of male victims/survivors of sexual violence, including boys and adult men.
- Facilitate the roll out of the GBV Treatment Protocol to private health facilities, including training of healthcare providers as outlined in recommendation four.
Recommendations to Donors
- Fund the development and implementation of standalone, specialised healthcare facilities for male victims/survivors of sexual violence most at risk (including those with diverse SOGIESC) such as the ones operationalized by YHDO.
- Fund health sector programmes targeting male victims/survivors of sexual violence that make linkages with other sectors, to ensure that the multiple and cumulative barriers facing male victims/survivors, including health, protection, livelihoods and justice barriers, are addressed.
INTRODUCTION
All Survivors Project (ASP) is an international non-governmental organisation (NGO) that supports global efforts to eradicate conflict-related sexual violence (CRSV) and strengthen national and international responses to it through research and action on CRSV against men and boys, including those with diverse sexual orientation, gender identity and /or expression and sex characteristics (SOGIESC), as well as other people with diverse SOGIESC. Since 2018, ASP has been working in Afghanistan with its partner Youth Health and Development Organization (YHDO) on research and advocacy related to CRSV against men and boys.
In 2020, ASP was awarded a grant to conduct research with YHDO on healthcare services and responses for male victims/survivors of sexual violence in Afghanistan. This forms parts of ASP’s wider work in Afghanistan to advocate for enhanced justice, legal, protection, livelihoods, health and psychosocial responses for male victims/survivors. Although ASP’s mandate focuses on CRSV against male victims/survivors, the research conducted extends to all forms of sexual violence against men and boys, including conflict-related and nonconflict-related sexual violence. This recognises that an enhanced health sector response in Afghanistan is required for all male victims/survivors.
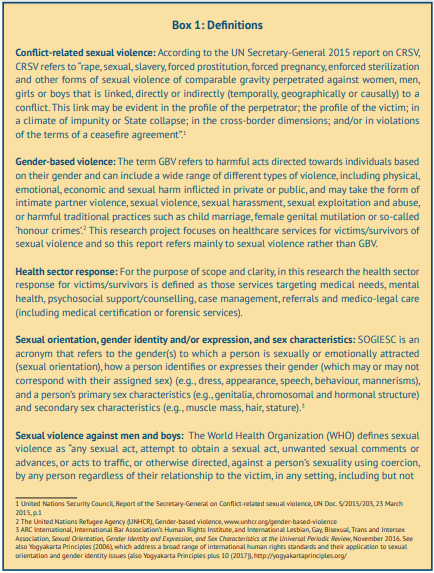
This report presents the key findings of the research and the recommendations made to the health sector, which will be used to support the development of a capacity-building tool for healthcare providers delivering services to male victims/survivors of sexual violence in Afghanistan. Throughout this report, a number of key terminologies are used and these are defined in Box 1. In line with ASP’s broader work, the report refers to male ‘victims/survivors’ of sexual violence, unless drawing from specific frameworks that use the term ‘survivor’ (such as the GBV Treatment Protocol for Healthcare Providers in Afghanistan). This framing recognises that not all men and boys who have experienced sexual violence view themselves as ‘having survived’ the abuse, and some may feel that they continue to be victimised. The term ‘victim/survivor’ acknowledges that people who have experienced sexual violence may identify themselves as a victim or as a survivor and that each individual has the right to choose the most appropriate language to express their individual experience.
Background
Gender-Based Violence in Afghanistan
Despite many gains made towards empowering Afghan women and girls in the last two decades, Afghanistan is still characterised by gender inequality, and women and girls experience widespread discrimination and abuses of human rights, including high levels of GBV. According to the Afghanistan Demographic and Health Survey conducted in 2015, 56% of ever-married women aged 15-49 had experienced physical, emotional or sexual intimate partner violence and this figure was as high as 92% in some provinces.[1] ‘Honour killing’ of women and girls is also practiced in Afghanistan, with 243 cases of ‘honour killings’ registered by the Afghanistan Independent Human Rights Commission between March 2011 and April 2013, with perpetrators predominantly identified as husbands or other male relatives.[2] Many ‘honour killings’ are reported to occur in response to suspicion of women committing or attempting to commit zina (sex out of wedlock, including adultery), with women often being accused of zina after experiencing rape or other forms of sexual violence.[3]
Although women and girls in Afghanistan are extremely vulnerable to violence, much less is known about the prevalence of violence against men and boys, particularly sexual violence. The Child Protection Action Network (CPAN) received reports of 108 cases of rape and sexual abuse against children in 2012, with boys comprising slightly less than half of these cases. In 2011, a slightly higher proportion of boys than girls reported sexual abuse or rape to CPAN.[4] However, it is unknown who the perpetrators were (i.e., parties to the conflict or other perpetrators) and thus whether these cases constituted CRSV.
The literature suggests that sexual violence against boys in Afghanistan often occurs in a conflict context, with government and anti-government armed actors being key perpetrators. In reports compiled from UN and other credible sources on CRSV in Afghanistan,[5] there is evidence of multiple cases of sexual violence against boys perpetrated by Afghan security forces and anti-government groups, including sexual abuse of boys through the practice of bacha bazi. According to the Law on Protection of Child Rights, bacha bazi, meaning ‘boy for play’, involves dressing male children in female clothing and keeping them for sexual pleasure and/or dancing or singing in public or private parties, and often involves rape, sexual touching, pornography or other forms of sexual violence.[6]
Sexual abuse of boys and young men occurs in other circumstances, including in education settings. A study on violence against children in schools found very high levels of sexual abuse against boys, with teachers and older boys reported to be the main perpetrators of rape of younger boys.[7] Similar findings were found in a more recent study that revealed widespread perceptions among boys that teachers and older students frequently perpetrated sexual violence against boys in school settings.[8] In recent months, allegations of sexual abuse of boys in schools in Logar Province have drawn attention to the vulnerability of boys to abuse in education settings.[9]
The evidence suggests that boys who experience sexual violence may be vulnerable to wrongful incarceration after being raped or sexually abused, often on charges of ‘moral crimes’ including pederasty or zina (sex outside of wedlock). An assessment by the UN Office on Drugs and Crime published in 2008 found that 14% of boys in detention had been charged with homosexual behaviour, with boys as young as 11 years old being charged with pederasty despite being victims of rape or other types of sexual violence perpetrated by older men.[10] Men and boys with diverse SOGIESC may be at particular risk of experiencing sexual abuse. In an assessment of adolescent experiences of sexual exploitation and abuse among men who have sex with men (MSM) in three provinces (Kabul, Kandahar and Balkh), 16 out of 36 adolescent MSM in Juvenile Rehabilitation Centres reported having had some experience of sexual assault with another male, whether as the victim/ survivor or perpetrator. [11] Vulnerability to abuse also occurs outside of these settings. A survey of MSM in Afghanistan found that 40% of those sampled reported having been raped by another man.[12] Reports of sexual violence were less common in another sample of MSM, 25% of whom reported having been forced to have sex in their sexual debut. However, 63% reported having negative feelings about this experience.
Health Sector Response
Afghanistan’s healthcare system is structured around the Basic Package of Health Services (BPHS) and the Essential Package of Hospital Services (EPHS), which comprise government health services and facilities predominantly run by NGOs. Under the BPHS and EPHS, healthcare services operate at three main levels. The first comprises community level services, delivered through health posts that are catchment areas for the outreach work of male and female trained volunteers referred to as community health workers (CHWs), or small static health facilities including health sub-centres (HSCs) and basic health centres (BHCs).[13] The second comprises district-level static health facilities located in larger communities or in district centres, including comprehensive health centres (CHCs) and district hospitals. The third level comprises provincial and regional hospitals.[14] The levels range from basic to more complete healthcare services, with an upward referral system under which more complex cases are referred to higher levels where there are larger numbers of healthcare staff, services and resources. Static facilities are supported by mobile health teams which perform outreach work in communities and provide additional opportunities for linking communities with the upwards referral structure. In addition to these different types of static and mobile health services overseen by the MoPH, some health facilities in Afghanistan are also run privately.
A range of services have also been developed specifically to address the health care needs of victims/survivors of GBV, although these are largely directed towards women and girls. Thirty-seven Family Protection Centres (FPCs) have been established in 26 provinces by the MoPH with support from UNFPA (the UN Population Fund) and implementing partners, and form part of a wider multi-sector response to a GBV programme that provides health, police and justice services for victims/survivors, with FPCs providing the primary entry point. FPCs are located in government provincial and regional hospitals to ensure their sustainability within the national health system, and provide support to victims/survivors, including basic health services, medical support, psychosocial counselling, legal support, help in collecting evidence and providing referrals to other services. Health focal points are available at the district level and refer GBV cases to the FPCs or other services, and FPCs conduct quarterly based coordination meetings with the health focal points. The MoPH, with the support of UNFPA, also has Women Friendly Health Spaces to identify GBV cases, provide support to victims/survivors and refer them to FPCs or other services. Despite these mechanisms to assist access to FPCs and other services, FPCs may not be accessible for all victims/survivors, particularly those who live in more remote locations. Consequently, some NGOs working in humanitarian response now send mobile outreach teams (comprising a psychosocial counselor, a community mobiliser and midwife) to visit communities and provide GBV services and referrals.[15] Although there has previously been resistance in Afghanistan to expanding CHW roles to respond to GBV,[16] it is recognised that, globally, CHWs are a key entry point to GBV health services for community members who cannot access formal services.[17] It is unknown, however, the extent to which CHWs in Afghanistan fulfill these functions.
Several resources have been developed to facilitate higher quality of health care provision for victims/ survivors of GBV, although, much like GBV services, these resources are largely directed towards women and girls. These include: a training manual for health professionals on a trauma-sensitive approach to care for victims/survivors of GBV in Afghanistan, developed in 2011 by medica mondiale and Medica Afghanistan; Standard Operating Procedures (SOPs) for Healthcare Sector Response to GBV, developed in 2013 by the MoPH and UNFPA; the GBV Treatment Protocol for Healthcare Providers in Afghanistan developed in 2014 by the MoPH, WHO and UN Women (GBV Treatment Protocol); and a comprehensive training package developed by WHO and UNFPA to train healthcare providers to use the GBV Treatment Protocol.
The GBV Treatment Protocol contains comprehensive information and guidance on a range of topics, including: legal frameworks and requirements, patient flow, confidentiality, documentation and reporting, survivor-centred care, identifying and responding to patient disclosures of GBV, and different types of care for victims/survivors. The Protocol is intended to provide guidance on healthcare response to all GBV victims/ survivors; however, although it notes that men and boys, particularly adolescent boys, can experience sexual exploitation and violence, the Protocol emphasizes that women and girls are disproportionately affected by GBV and the Protocol is largely targeted towards them. There are some sections of the Protocol that explicitly refer to the provision of services for men and boys; however, there are also a number of gaps in this regard, as articulated in this report.[18]
Despite the development of the BPHS and EPHS, and specialised services and resources for victims/survivors of GBV, there are persistent barriers to female victims/survivors accessing healthcare services in Afghanistan and these are well documented in the literature.[19] However, very little is known about the barriers that men and boys face accessing GBV services following experiences of sexual violence. An MoPH psychosocial counselling training package on GBV suggests that male victims/survivors of rape are much less likely to report the incident or seek health care due to feelings of embarrassment.[20] The GBV Treatment Protocol also has a brief section on men, which notes that male victims/survivors of GBV are unlikely to seek medical attention unless they have had severe injuries, in part due to the stigma and cultural sensitivities around sexual violence against men. The Protocol also notes that men presenting to healthcare providers after experiencing rape may be concerned about their masculinity, sexuality, inability to prevent the assault, or the opinions of others who may think they are homosexual.
Research on Male Victims/Survivors of Sexual Violence
In order to address the large gaps in knowledge about male victims/survivors of sexual violence in Afghanistan and the barriers they face accessing quality healthcare provision, ASP and YHDO conducted research in 2020. The objectives of the research were to:
- Understand the healthcare experiences and needs of male victims/survivors of sexual violence and the barriers to their access to quality healthcare services.
- Understand the practices of healthcare providers in relation to supporting male victims/survivors of sexual violence and the barriers they face in providing quality healthcare services to them.
- Understand what a survivor-centred approach to healthcare provision means, and how it is applied in Afghanistan, with regards to male victims/survivors.
- Develop a set of recommendations for enhanced survivor-centred healthcare services for male victims survivors of sexual violence that will be used to develop a tool for the health sector.
OVERVIEW OF METHODOLOGY
This section provides an overview of the methodology and methods employed for the research: a full description is included in Annex A.
The research was conducted in three provinces: Kabul, Balkh and Kandahar. These provinces were not selected on the basis of estimates of the prevalence of sexual violence against men and boys.[21] Rather, they were selected in order to capture data from three geographical regions of the country (central, northern and southern) and also because of YHDO’s presence in these regions. Data collection was conducted between August and November 2020.
The overall research approach was qualitative, with four key methods employed:
- Desk review: A desk review was conducted, including literature on sexual violence against men and boys and the health sector response, with a focus on evidence from Afghanistan. A list of selected documents is provided at the end of this report, with URLs where available.
- Stakeholder mapping: A stakeholder mapping was conducted to identify existing systems of healthcare response that include coverage of male victims/survivors, predominantly through a desk review of online documents.
- Key informant interviews with stakeholders: From the stakeholder mapping, a selection of stakeholders were invited to participate in key informant interviews (KIIs). Ten interviews were conducted with a range of individuals, including government stakeholders, and staff from national and international NGOs and UN agencies.
- In-depth interviews: In-depth interviews (IDIs) were conducted with 27 male victims/survivors of sexual violence, 44 healthcare providers working in different types of static health care facilities, and 26 community health workers, with a total of 97 IDIs conducted.
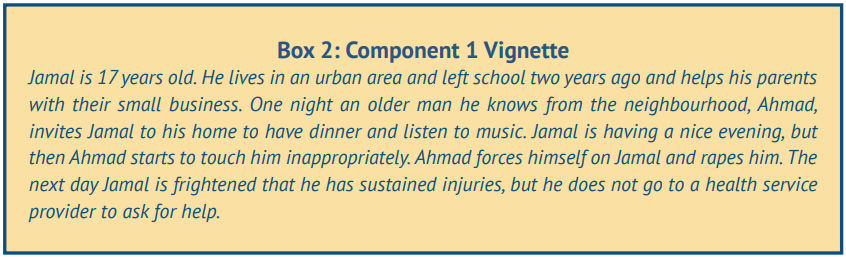
IDIs were based on a storytelling approach in which a vignette/story of a male victim/survivor of sexual violence was used to prompt storytelling and discussion whereby different types of participant were asked to discuss the story through the eyes of the victim/survivor. Three different qualitative tools were developed for each type of participant (male victims/survivors, healthcare providers, and community health workers), and all three were harmonised to draw from the same approach. All three tools were divided into three components:
- A vignette of a hypothetical scenario involving sexual violence perpetrated against a 17-year-old boy who does not access health services (see Box 2) and questions or probes about why he does not want to do so and the barriers that he might face if he does.
- A continuation of the vignette to facilitate a walk through a healthcare pathway to explore what occurs when a victim/survivor accesses services at a healthcare facility or through a community health worker.
- A series of questions about participants’ own experiences accessing healthcare after experiencing sexual violence (for victims/survivors) or delivering healthcare services (healthcare providers and community health workers) and what is needed to improve healthcare response for male victims/ survivors.
These three components are described more fully in Annex A, and the tools are included in Annex B.
Due to the COVID-19 pandemic, all data collection was done remotely through telephone interviews. The research team had concerns about how to ensure the confidentiality and privacy of male victims/survivors when engaging in telephone interviews. Consequently, in order to mitigate risks, a hybrid approach was employed whereby victims/survivors were supported to access a YHDO office where they were provided with a safe, private and COVID-19 sterilised space with the necessary technology to participate in an interview facilitated remotely.
The research was conducted in line with an ethical, safe and survivor-centred approach.
- Ethical approval was obtained from the Institutional Review Board of the MoPH in Afghanistan.
- No male victims/survivors under the age of 18 were sampled for the research.
- All participants were required to provide informed consent before participating in interviews.
- Confidentiality for participants was ensured by de-identifying transcripts and removing names, names of healthcare facilities or organisations and district names from the report.
- In order to handle victim/survivors’ possible distress and re-traumatization, YHDO had counsellors available to provide services.
- The research team participated in ethics and safety training, including on ensuring privacy and confidentiality, obtaining informed consent without coercion, respecting the withdrawal of consent at any time, ensuring respect for victims/survivors at all times, recognising signs of distress and handling disclosures of violence.
The research team faced a number of challenges implementing the research, leading to some limitations. See Annex A for a more extensive discussion of challenges and limitations, with the main ones listed below.
- Only seven male victims/survivors (one quarter of those interviewed) reported having accessed non-YHDO healthcare facilities for sexual violence they had experienced in the past. Further, only nine healthcare providers (one fifth of those interviewed) reported having provided services to male victims/survivors of sexual violence. This challenge was expected and difficult to avoid given the substantial barriers male victims/survivors face accessing healthcare services and was one of the reasons for using a hypothetical vignette approach in the interview tools. Consequently, much of the data is based on perceptions or, in the case of victims/survivors, what they had heard from other victims/survivors, rather than on their own direct personal experience.
- Only one CHW reported having provided support to male victims/survivors. Although the CHW data was useful insofar as CHWs are widely recognised as a possible entry point to male victim/survivors’ access to healthcare facilities through referrals, CHWs had little awareness or knowledge about male victims/survivors of sexual violence or their needs.
- Given that all victims/survivors interviewed were adults, there is an important gap in the research on the experiences of boys. The research team was able to analyse some data retrospectively where adult men disclosed that they had experienced sexual violence at a young age. Further, of the nine cases in which healthcare providers reported that they had provided services to male victims/survivors in the past, five referred to providing services to boys, also allowing additional learning about healthcare response to boy victims/survivors of sexual violence. However, the lack of direct data collected on child and adolescent boy experiences of accessing healthcare services is a gap that is important to address in future research.
RESULTS
Barriers to Male Victims/Survivors of Sexual Violence Accessing Healthcare Services
The research has identified a number of barriers that prevent male victims/survivors of sexual violence from accessing healthcare services. Following a social ecological model of public health,[22] this section presents these barriers according to five different levels: (1) individual barriers, (2) interpersonal barriers (3) community-level barriers, (4) organisational barriers and (5) structural barriers. It should be noted that these barriers do not operate in isolation and male victims/survivors face multiple, mutually reinforcing barriers, making access to healthcare services extremely challenging.
Lack of Knowledge or Awareness
At the individual level, lack of knowledge or awareness emerged as a barrier to male victim/survivors’ access to healthcare. This barrier was described in different ways by male victims/survivors and healthcare providers but in both groups age was implicated, and this barrier was framed as one particularly facing younger boys.
Male victims/survivors suggested that lack of awareness of how to access a healthcare facility, including lack of knowledge about their location and what services are available, was a key barrier. They emphasized that younger boys would be unlikely to understand how to access a healthcare facility or to have the autonomy to do so, and victims/survivors who had first experienced sexual abuse as a child noted being unaware of how to access healthcare facilities. In contrast, older adolescent boys and adult men were perceived to have greater awareness of available services and the mobility to reach them. Healthcare providers also expressed awareness that boys were likely to have limited knowledge of how to access a facility or that these services existed and were reliant on caregivers to facilitate access.
Healthcare providers raised the issue of children’s lack of knowledge about their bodies and inappropriate sexual touching, and that children may not understand that they have been sexually abused. Approximately a quarter of healthcare providers interviewed for the research raised the lack of appropriate sex and relationship education in Afghanistan as a key driver of sexual violence against boys. In cases where this issue was raised, healthcare providers emphasized that both boys and girls needed to learn how to protect themselves from sexual violence by acquiring information about their bodies, including their sexual organs and how to recognise inappropriate (sexual) attention or touching. In most cases, families were perceived to be the most appropriate actors to deliver this education to their children. However, a small number of healthcare providers (three) emphasized that Afghanistan’s education system was a more appropriate system through which to deliver sex and relationship education. In recent years, academics and international organisations working in Afghanistan have advocated for the inclusion of comprehensive sexuality education, often referred to as Family Life Education (FLE), to be included in the national curriculum.[23] Although the MoPH with support from UNFPA has developed and handed over a series of FLE materials to the MoE[24], these are yet to be integrated into the national curriculum.
Despite participants suggesting that adult men were more likely to know how to access a healthcare facility, the results of the research suggest that victims/survivors may lack knowledge of the type and quality of care they will receive. There was significant dissonance between healthcare provider descriptions of the care they would provide to a male victim/survivor, and the treatment that male victims/survivors expect to receive (see further details in the sections of this report on healthcare services for male victims/survivors of sexual violence and the needs of male victims/survivors). Although this may be due in part to some persisting gaps in the capacity of healthcare providers to deliver services to male victims/survivors, it is also possible that victims/survivors are unaware of existing protocols (e.g., confidentiality protocols) and how the health sector has grown more generally in relation to GBV response (for instance, with the roll out of the GBV Treatment Protocol and the establishment of FPCs).
Social Stigma
Social stigma has been found to be a significant barrier to male victim/survivors’ help-seeking in a number of different country contexts, including in conflict and humanitarian settings. Several studies have emphasized male victim/survivors’ fears of social stigma from family and community members and the emotional abuse and mistreatment that they would experience if their victimization is known to others in their community or family. [25]
In data collected for this study, almost all the male victims/survivors interviewed referred to social stigma and subsequent shame or loss of dignity as the most important barrier they faced in seeking help from a healthcare facility. A common theme was the poor treatment of victims/survivors by community members, who were reported to tease, taunt and humiliate victims/survivors due the violence they had experienced. Victims/survivors described many negative impacts of this poor treatment from community members, including feelings of rejection and social isolation and the subsequent negative impacts on mental health, in some cases leading to suicidal thoughts. Victims/survivors noted that stigmatising attitudes and behaviours from community members, including peers, may lead them to drop out of school or leave their communities to escape mistreatment. Victims/survivors also described the negative impact that stigma has on the honour and reputation of their families, and suggested that preserving their families’ dignity was a key reason for decisions not to seek help. Victims/survivors suggested that families may also need to relocate to a different community to escape stigma and shame.
Victim/survivors’ perceptions of sources of stigma are closely linked to ‘blame the victim’ discourses whereby the source of stigma is perceived to be the assumption that victims/survivors are responsible for the violence they experienced. Just over 50% of the male victims/survivors and approximately 15% of the healthcare providers and CHWs sampled for the research reproduced a ‘blame the victim’ discourse. Victim blaming is a common community response to all victims/survivors of sexual violence, including male and female victims/survivors, and is often linked to preserving the power and privilege of perpetrators and social norms that justify violence.
The majority of participants who reproduced a ‘blame the victim’ discourse (approximately three quarters of male victims/survivors and healthcare providers, and all CHWs) suggested that victims/survivors should have ‘known better’ and were to blame for making a decision to enter a situation perceived to be risky. While participants often recognised that victims/survivors may have been deceived by perpetrators, victims/ survivors were still perceived to be at fault for the situation arising at all.
The second type of ‘blame the victim’ discourse was that if a risky situation could not be avoided, then it was the responsibility of the victim/survivor to defend himself or escape the situation. This discourse was only used by four male victims/survivors.
The third type of ‘blame the victim’ discourse was that the victim/survivor must have wanted sexual engagement and so the sexual act would have been consensual. Only three victims/survivors and one healthcare provider reproduced this type of discourse, which was linked to the previous two discourses insofar as victims/ survivors were presumed to have consented to sexual engagement if they (a) entered a situation assumed to be risky and/or (b) did not attempt to run away or defend themselves (or were not successful in doing so). This ‘blame the victim’ discourse was linked to the perceptions of victim/survivors’ SOGIESC. Where the victim/survivor in the hypothetical vignette was positioned as having a diverse SOGIESC, including being gay or transgender, there were assumptions that he may have welcomed the sexual violence.
These three ‘blame the victim’ discourses were largely targeted toward adult male victims/survivors, suggesting that age is an important factor in how people perceive the role of men and boys in negotiating risk of sexual violence, and the subsequent stigmatisation of victims/survivors if they are unable to negotiate this risk. Younger boys are perceived to suffer less stigma due to assumptions that they are less able to understand the consequences of being in situations that could heighten risk of sexual violence, are unable to defend themselves, have no sexual desire and are unable to consent to sexual relations. In contrast, adult men are presumed to be able to avoid, or defend themselves from, sexual violence and are thus blamed for the violence they experience. According to victims/survivors, in general, stigma is less pronounced for younger boys, and families are more likely to facilitate boys’ access to a healthcare facility. However, as the age of boys increases, families are perceived to be less likely to support their access to healthcare due to greater stigma and shame.
It is important to note that ‘blame the victim’ discourses were reproduced more by victims/survivors than by healthcare providers or CHWs. There are a number of reasons why this might be the case. It is possible that male victims/survivors direct stigma and blame onto other male victims/survivors as they have internalized the stigma and blame they have received from others. For instance, there is evidence in other settings that male victims/survivors may internalize negative attitudes, beliefs and stigma, although this usually occurs through self-blame rather than blaming other men or boys.[26] It is also possible that male victim/survivors’ past experiences of sexual violence have led to deep feelings of suspicion of other men, including those who may be perpetrators, which is a documented impact of sexual violence on some men and boys.[27] This was particularly evident in victim/survivors’ reproduction of the first type of ‘blame the victim’ discourse, whereby they stressed that all men and boys should be discerning about accepting social invitations from other men, particularly at night.
Although fewer healthcare providers and CHWs reproduced ‘blame the victim’ discourses, it is interesting to note that those who did were all male. This could be due to a bias in the sample given that there were more male than female healthcare providers and CHWs interviewed for the research. However, it is also possible that there is a gender dimension to discourses that stigmatise and blame men and boys, including among victims/survivors themselves. Research participants did not explicitly refer to masculinity or what it means to be a man in Afghan society. However, perceptions that men and boys are responsible for controlling their social environment and defending themselves from risk, including physically defending themselves, may point towards models of masculinities that male research participants in particular reproduce.
Threats of Violence and Abuse
Victim/survivors’ fears of experiencing emotional abuse, including being teased or taunted by community members, emerged as a significant barrier to their access to healthcare services. However, a number of victims/survivors also reported fears of experiencing threats of physical violence if they disclosed their experience to a healthcare provider.
When research participants referred to threats of physical violence against victims/survivors, they emphasized the risk of threats from perpetrators who might fear the disclosure of their identity to healthcare providers who may then refer the case to judicial actors. There were widespread perceptions that disclosing cases of violence to healthcare providers could create additional problems for victims/survivors if perpetrators of sexual violence retaliated against victims/survivors or their families. Victims/survivors from all three provinces stressed how threats from perpetrators would be more pronounced if they were armed actors or other types of powerful actors. Victims/survivors emphasized the greater threat of physical violence, including murder, to themselves and their families if perpetrators were armed. This may occur through verbal threats of violence to force victims/survivors to remain silent or direct acts of physical violence if a victim/ survivor’s case is reported to the judiciary via a healthcare facility. Several victims/survivors also suggested that perpetrators of sexual violence would not necessarily make physical threats, but may blackmail victims/ survivors and pressure them to stay silent; for instance, by threatening to show video or photographs of the rape to relatives or to post them on the internet or social media.
Despite concerns about perpetrators threatening victims/survivors being common, male victims/survivors of sexual violence frequently referred to physical threats from their own family members. A third of victims/ survivors interviewed for the research, particularly those in Kandahar and Kabul, suggested that families might beat or even kill victims/survivors if the family is perceived to be dishonoured or shamed. Several victims/survivors also referred to fears of family members throwing them out of the house or forcing them to leave their community.
Although the types of fears outlined above were common in male victim/survivors’ narratives, it is interesting to note that healthcare providers perceived threats of physical violence or murder in the name of ‘honour’ to be a problem faced mainly by female victims/survivors. Healthcare providers highlighted the importance of girls’ virginity in Afghan culture and the negative repercussions on women and girls if they are raped given they become less marriable, leading to perceptions of shame and dishonour in the family. However, there was less recognition that male victims/survivors might also be punished through violence, partly due to perceptions that the shame would be less given that men and boys would presumably be able to marry in the future.
Conflict
Almost all of the participants interviewed for the research recognised that perpetrators of sexual violence against men and boys, particularly bacha bazi, are often armed actors, including government and nongovernment armed actors and armed warlords. As noted in the previous section, victims/survivors emphasized how threats from perpetrators, including threats of physical violence and murder (both to themselves and their families), were particularly strong barriers to accessing healthcare services in cases where perpetrators were armed actors. These barriers were largely linked to concerns about cases being referred from healthcare facilities to judicial actors, and the subsequent risks that this would pose to survivors and their families if armed actors retaliated against them.
Despite overall recognition that perpetrators of sexual violence against men and boys are often armed actors, few research participants emphasized power in conflict as a driver of sexual violence against men and boys. Healthcare providers and CHWs in particular perceived armed actors to perpetrate sexual violence due to lack of education. Three quarters of healthcare providers and CHWs who referred to armed actors suggested that they were illiterate, had not received an appropriate Islamic education or were not sufficiently knowledgeable about national laws, international human rights laws or Sharia laws that prohibit sexual violence. These perceptions were accompanied by assumptions that if armed perpetrators were adequately educated, they would not perpetrate sexual violence against men and boys.
In the limited cases in which conflict drivers were more explicitly stated, research participants referred to conflict-driven displacement of boys putting them at risk of sexual violence, including where displacement led boys to join non-government armed groups. Other conflict drivers mentioned included the death of boys’ family members as a result of conflict, leading them to work to support their households, including in situations that put them at heightened risk of sexual violence (e.g., sex work or street work). Only a few participants (four healthcare providers), suggested that weak rule of law (rather than the educational level of perpetrators) was a key conflict driver of sexual violence against men and boys. These participants highlighted the impunity of powerful perpetrators and their connections with government officials (or in many cases perpetrators belonging to government entities) as being a more significant factor in CRSV.
Poverty and Economic Vulnerability
In Afghanistan, poverty is a recognised barrier to access to healthcare services more generally,[28] and a barrier that women and girl victims/survivors of GBV also face, including lack of funds to pay for transport (especially if living in remote and rural locations) or medical service fees.[29] The research suggests that male victims/survivors of sexual violence may also face economic barriers to accessing healthcare services. Just over three quarters of participants, particularly healthcare providers, emphasised economic barriers to access to healthcare services. There was some variation in perceptions of the types of economic barriers male victims/survivors might face. Most healthcare providers highlighted that services in government healthcare facilities under the BPHS and EPHS were free and that lack of money should not pose a significant economic barrier in this regard. Although victims/survivors also made reference to government facilities offering free services, several suggested that payment for government services was sometimes required. It is possible that some victims/survivors lack awareness of the free nature of primary health services captured under the BPHS and EPHS. However, it is also possible that they are referring to services that are not covered by the BPHS and EPHS.
Despite general recognition that victims/survivors could access free healthcare services in government facilities, both victim/survivors and healthcare providers cited economic problems associated with access to available government facilities. In particular, they highlighted how difficult it was for victims/survivors with poor socio-economic status living in rural or remote areas to pay for transport to access a healthcare facility at the district level or in the provincial centre. Victims/survivors noted this barrier more in relation to hypothetical scenarios involving other male victims/survivors rather than their own experiences, which is likely due to victims/survivors being sampled in urban settings where transport is more readily available. Nevertheless, victims/survivors reported other types of economic barriers, including lack of provision of medications, which those from poor families were unable to afford, despite BPHS facilities providing essential medications for patients. This suggests that victims/survivors may not have adequate information about the provision of services in government facilities.
References to lack of money for transportation and to purchase medicines were particularly common in Kandahar. In cases where victims/survivors recognised that government healthcare services were free, several suggested that the quality of services were poor and that victims/survivors were better off accessing private facilities, which are perceived to have better quality services, including stricter confidentiality. However, private facilities are perceived to be unaffordable for poorer families. One healthcare provider in a private facility referred to a charity section that delivered free services to patients who were poor, and there are some private facilities that have mechanisms in place to reduce costs for poor families; however, it is possible that male victims/survivors are unaware of these mechanisms for support.
Poverty and economic vulnerability were not only described as key barriers to healthcare access, but were also described as key drivers of sexual violence against men and boys. Research participants perceived sexual violence to occur when families failed to safeguard sons, and this failure was directly linked to poverty and economic vulnerability. A common way in which families, particularly parents, are perceived to have failed to safeguard male children is through perceptions that they have insufficient oversight of their children, with parents described as often too busy working to be aware of what their sons were doing. Another way that families are believed to have failed to safeguard sons is related to perceptions that poor families may increase the vulnerability of boys by putting them in situations of risk. In some cases, participants suggested that families might actively do so by encouraging or forcing them to participate in labour that might leave them vulnerable to participation in sex work or practices associated with sexual exploitation and abuse, including bacha bazi. However, the majority of research participants suggested that families were to blame in a more indirect way by forcing boys to drop out of school and/or participate in child labour, with street working boys perceived to be at particular risk of sexual violence.
Economic factors were not always depicted as the fault or responsibility of victim/survivors’ family members. Two male victims/survivors and one male CHW actively positioned perpetrators of bacha bazi as responsible for economically and sexually exploiting boys due to the poverty of their families. Some research participants (eight male victims/survivors, five healthcare providers and four CHWs), particularly in Kandahar, depicted male victims/survivors as more active agents seeking economic activity or independence. In most of these cases, research participants did not reproduce ‘blame the victim’ discourses but rather suggested that perpetrators deceived boys and men by preying on their economic needs and providing them with economic assistance.
Perpetrators’ exploitation of victim/survivors’ ‘weakness’ was a theme that emerged across a number of interviews; however, ‘weakness’ was not always defined in relation to economic need or poverty. Several victims/survivors referred to boys and men wanting or needing other forms of support that perpetrators might provide, including social networks or access to employment, or that perpetrators might entice boys with gifts, including mobile phones or clothes, or social status. The formation of these relationships was perceived to lock boys and men into economically dependent relationships with perpetrators that would inevitably be accompanied by or end in sexual violence.
Availability of Services
Only three research participants across the whole sample stated that lack of facilities was a barrier to male victims/survivors seeking healthcare services, and there were widespread perceptions among healthcare providers in particular that the BPHS was largely successful in reaching the population at the community level, including victims/survivors of violence. Nevertheless, there was widespread recognition that there was a lack of specialised services for this particular group. Male victims/survivors emphasized their preference for a healthcare facility that had specialised capacity to assist men and boys, and particularly a preference for private, non-public health facilities due to the barriers already noted, including perceptions that private healthcare facilities had higher quality care and better confidentiality procedures.
A number of healthcare providers suggested that GBV procedures and protocols would be easier to manage if healthcare facilities had a specific department for GBV cases, and both victims/survivors and healthcare providers suggested that facilities would benefit from having a section focused on delivery of services for men and boys who had experienced sexual violence. Few healthcare providers spoke about how such a department would function in a way that would protect the privacy of victims/survivors and avoid stigmatisation of those actively seeking services. One healthcare provider noted that any department tasked with providing services to victims/survivors of GBV, whether female or male, should not be visibly marked as such in order to respect confidentiality and privacy, which is in line with recommendations made in the GBV Treatment Protocol. However, one healthcare provider suggested that “the GBV services room should have a signboard to be visible for everyone without asking about it” and another suggested that such signboards were present in their own facility, suggesting that not all providers understand the implications of stigma for victims/ survivors and the harm of visibly labelling GBV services.
One stakeholder from a UN organisation suggested that specific health centres should be established to directly target ‘men with high-risk behaviours’ given they are from a particularly vulnerable group that experiences heightened stigma. Others suggested that existing healthcare facilities could be expanded to meet the needs of male victims/survivors. For instance, FPCs, which are typically located in provincial or regional hospitals, do serve the function of targeting services specifically to victims/survivors of GBV. However, there were some conflicting perspectives on the extent to which FPCs can or do provide support to male victims/survivors of sexual violence. One FPC focal point in Kandahar suggested that the FPC only provided services for women and girls, and that there were no parallel centres for men and boys. However, two stakeholders interviewed for the research, one from the MoPH and another from an NGO running an FPC in Kabul, stressed that the mandate of FPCs was to deliver services to any victim/survivor of GBV. Nevertheless, stakeholders emphasized that given FPC staff are all female, it is rare that male victims/survivors would approach an FPC seeking assistance and in almost all cases they would be boys (although men may also come to an FPC asking for assistance, they would be referred to other healthcare facilities with male staff). According to the stakeholder interview with an MoPH focal point, 70 cases of sexual violence against male victims/survivors were registered in FPCs between 2013 and 2020. An FPC focal point in Kabul also noted that they had received cases from male victims/survivors of sexual assault in the past, although not more recently in 2020. This focal point reported that the FPC referred male victims/survivors to YHDO and that the lack of male victims/survivors attending the FPC in 2020 could be because these men and boys in Kabul are now aware of YHDO services and seek them directly.
Stigma From and Negative Attitudes of Healthcare Providers
It is well documented in Afghanistan that a significant barrier to women and girl victims/survivors accessing health services is the negative and stigmatising attitudes that healthcare providers might direct towards them.[30] Although there is no data available on healthcare providers’ attitudes and behaviours towards male victims/survivors of sexual violence in Afghanistan, the global evidence suggests that negative attitudes of healthcare providers, including using humiliating, blaming and stigmatising language, are a significant barrier to victim/survivors’ healthcare access.[31]
The victims/survivors interviewed for this research also reported fear of stigma, blame and negative attitudes from healthcare providers as a barrier to accessing healthcare services. Victim/survivors’ concerns about being stigmatised and blamed by healthcare providers are mostly in line with the ‘blame the victim’ discourses, outlined previously: the victim/survivor should have ‘known better’; the victim/survivor must have developed inappropriate social engagements; the victim/survivor should have defended himself; or the victim/survivor must have wanted sexual engagement. In addition, two victims/survivors suggested that poor treatment from healthcare providers, including blame and judgement, may be due to concerns that stigma might somehow affect the facility and bring the ‘dignity’ of the facility into disrepute.
Victim/survivors’ fears of being blamed or judged by healthcare providers appear to be particularly pronounced among male victims/survivors with diverse SOGIESC. Victims/survivors referred to the specific visibility of those with diverse SOGIESC, and the verbal abuse that they would face if attempting to access a healthcare facility. For instance, one victim/survivor from Kabul described how the recognition of a transgender victim/ survivor’s gender expression as ‘different’ would be linked to abusive behaviour from multiple staff along the care pathway, and even before the victim/survivor reaches the healthcare facility.
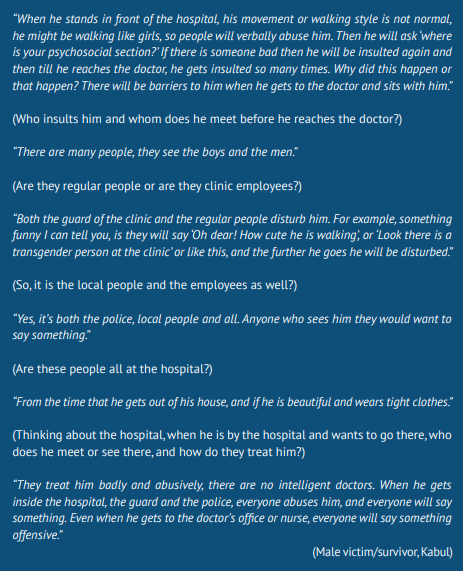
This extract has a number of important implications. One is that stigmatising behaviour towards victims/ survivors begins well before they arrive at a healthcare facility. Further, although healthcare providers deemphasized the role or importance of guards or initial clinic focal points in providing services to victims/ survivors of violence, the fears of male victims/survivors with diverse SOGIESC illustrate how stigmatising treatment from initial clinic focal points can discourage victims/survivors from attempting to access a healthcare facility. Another implication is that regardless of how a victim/survivor with diverse SOGIESC is treated by a medical practitioner, by the time he reaches that point in the care pathway trust in care is likely to have diminished.
Healthcare providers rarely made any reference to male victims/survivors with diverse SOGIESC; however, they did appear to be aware of general fears that male victims/survivors had of the negative attitudes of healthcare providers. Five healthcare providers admitted that some providers might stigmatise or even criminalise victim/survivors’ experiences of sexual violence. However, almost all insisted that healthcare providers do not behave in these ways, although there are some exceptions (see further detail in the section of this report on healthcare services for male victims/survivors).
One way that healthcare providers do clearly reproduce negative attitudes about victims/survivors of violence is in their support of certain misconceptions or rape myths about the perpetration of violence. In Afghanistan, such misconceptions have been documented in relation to healthcare provider attitudes about female GBV victims/survivors. But little has been documented in relation to myths about male victims/survivors of sexual violence. In a 2015 baseline evaluation, 26% of healthcare providers believed that men could not be survivors of rape and this was as high as 40% in Balkh Province and 50% in Bamyan Province, although fewer healthcare providers in Kabul (13%) disagreed with the statement.[32] In a more recent study of the GBV Treatment Protocol roll out in 14 new provinces, 39% of healthcare providers believed that men cannot be victims of rape.[33] An interesting finding to emerge from this study was that most healthcare providers failed to inform female patients about their rights in relation to GBV. However, the strongest predictor of healthcare providers informing female patients about GBV and their rights was an understanding that men could be raped.
In the ASP study, all healthcare providers seemed aware that men and boys could experience sexual violence; however, they reproduced other types of rape myths. One was that the impacts of rape on men and boys were not as severe as for women and girls, despite global evidence that men and boys can be deeply affected by rape, including both physically and psychologically.[34] Another common rape myth reproduced by healthcare providers was a justification for perpetrators’ behaviours through beliefs that men’s uncontrollable sexual desire is the key cause of sexual violence against men and boys. Uncontrollable sexual desire of perpetrators of sexual violence against men and boys in Afghanistan is perceived to be largely rooted in certain social and cultural practices and norms. One is the high cost of weddings preventing men from marrying, and another is the cultural and religious segregation of men and women, both of which are believed to lead to men raping other men and boys in order to release their sexual impulses. One victim/survivor also suggested that some perpetrators may have same-sex sexual desire, leading them to rape men and boys if they cannot express their desire in a consensual relationship. Regardless of the object of desire, the rape myth of uncontrollable sexual desire circulated extensively across the data, particularly among healthcare providers, a quarter of whom referred to this particular driver of sexual violence against men and boys. In contrast, only three victims/survivors and one CHW made the same references.
In relation to beliefs about rape associated with the high cost of weddings, which assumes that the perpetrator does not have sufficient economic capital to pay for his wedding, research participants did not acknowledge an apparent contradiction in this explanation. The majority of research participants recognised that perpetrators of sexual violence against men and boys are often powerful and wealthy actors, including armed actors. Yet they still reproduced rape myths about men’s uncontrollable sexual desire due to the unaffordability of weddings as a key driver of sexual violence against men and boys, despite married men also being likely perpetrators. Only a few research participants acknowledged that perpetrators may in fact be married, in some cases with multiple wives, although one of these participants also suggested that married men might rape men and boys if unhappy with sexual relations within their own marriage, again relying on the rape myth of uncontrollable sexual desire to explain why men rape other men or boys.
Lack of Confidentiality Protocols
Concerns about stigma and shame are closely linked to victim/survivors’ fears of confidentiality breaches if they access healthcare facilities. One of the greatest fears that victims/survivors described was that healthcare providers would disclose the violence to families or others in the community. A number of victims/survivors suggested that fears of confidentiality breaches, particularly to family and community members, are less pronounced when accessing private health facilities, and there were widespread perceptions that healthcare providers in private facilities were more likely to respect confidentiality and not disclose the case. These perceptions were linked to a more general view that private facilities have better quality services, albeit more expensive services that many victims/survivors would not be able to afford. Several victims/survivors suggested that there was more anonymity in private facilities and that accessing government facilities could carry more risk as they are more rooted in community social networks. Subsequent fears include known community members attending the health facility, seeing victims/survivors and somehow finding out about their case, or healthcare providers being more likely to know one another and victim/survivors’ families and members of their community and breaching confidentiality through personal networks.
When asked to describe any formal procedures or protocols in their health facility for dealing with cases of sexual violence against men and boys, most healthcare providers did describe various internal procedures or requirements for documentation when dealing with GBV cases in general, albeit mainly with women and girls. These included confidentiality procedures for the recording and handling of data, including the use of ID codes and safe storage of data, and the use of consent forms and referral forms to refer victims/survivors to additional services. Healthcare providers in smaller facilities, particularly BHCs, were less familiar with internal procedures and several stated that no formal GBV procedures or protocols existed in their health facility.
Lack of Healthcare Provider Capacity
Despite references to confidentiality, consent and referral protocols in larger health facilities, all healthcare providers interviewed for the research either stated that their healthcare facility did not have any specific protocols for how to deal with cases of sexual violence against men and boys, or that they did not know if such a protocol existed. Several healthcare providers noted that there were protocols for dealing with cases of sexual violence against women and girls, or protocols that addressed the needs of victims/survivors of violence in general, but that there was little specific guidance on dealing with cases of men and boys. Stakeholders interviewed for the research who are supporting BPHS implementation also confirmed that there were no protocols within healthcare facilities for how to address sexual violence against men and boys. One stakeholder suggested that although individual healthcare facilities might have their own SOP, there was no centralised protocol or SOP within the BPHS and EPHS specifically related to male victims/survivors, and that healthcare facilities would welcome the MoPH’s lead in establishing a more centralised protocol.
Where healthcare providers referred to GBV protocols, it is likely that they were referring to the GBV Treatment Protocol for Healthcare Providers in Afghanistan, which does contain some, albeit limited, direct reference to men and boys. When asked specifically if they knew of the GBV Treatment Protocol or had received training in it, 22 healthcare providers (just under half of those interviewed) said that they were familiar with the Protocol or had heard of it, and 15 said that they had participated in training on the Protocol, including three female and 12 male healthcare providers. Healthcare providers who had heard of the Protocol but had not participated in the training noted that other colleagues had participated; however, they also suggested that the training should be disseminated more widely in order to ensure capacity in GBV service provision was distributed across all relevant staff. Of those who had participated in training, only three remembered any specific content related to male victims/survivors. There was a strong appetite from healthcare providers to receive training on how to deliver services to male victims/survivors of sexual violence, particularly from those providers who had not participated in any such trainings or any GBV trainings at all. There was particularly strong interest in training from healthcare providers in smaller health facilities and private health facilities, perhaps due to the GBV Treatment Protocol training being focused in provincial and regional hospitals.
Fear of Sexual Abuse From Healthcare Providers
As described previously, fear of threats and further violence from perpetrators or family members is a strong barrier to male victims/survivors seeking healthcare services. However, they do not only fear further violence from perpetrators and family members. Victim/survivors also referred to the fear that male healthcare providers might perpetrate sexual violence against them. Although no victims/survivors interviewed for the research claimed that they had been raped by a healthcare provider, several told stories of friends who had experienced sexual violence at the hands of a healthcare provider or expressed fear that this could be the outcome of accessing a health facility. Victims/survivors also referred to fears of other types of mistreatment or sexual abuse if healthcare providers identified them as having a diverse SOGIESC. One victim/survivor in Kabul suggested that a healthcare provider might attempt to look at a victim/survivor’s genitalia to confirm suspicions about his transgender expression or identity (“I told you, if he looks like girls the doctors will try to look at his private parts”), and may expel him from the healthcare facility.
Laws and Policies
In Afghanistan, there is no legal requirement to mandatorily report cases of sexual violence or other types of GBV.[35] Nevertheless, male victims/survivors reported strong fears that healthcare providers might disclose their case to actors in the judicial system, including police or other justice actors, without their consent, and this fear is a strong deterrent to male victims/survivors approaching healthcare facilities for support. These fears are likely linked to the complex legal environment for male victims/survivors in Afghanistan, particularly for adult men, whereby rape, including of men and boys is illegal, but where same-sex sexual acts are also criminalised.
The legal and policy environment for addressing GBV against women and girls in Afghanistan has developed substantially in the last decade with the implementation of the Elimination of Violence against Women (EVAW) Law adopted in 2009 (although the EVAW Law remains based on Presidential decree rather than ratified in Parliament).[36] The legal and policy environment to address violence against children, including boys, has also shifted more recently. The revised Penal Code, which came into force in 2018, contains a chapter on the criminalisation of bacha bazi, including participation in any events involving bacha bazi (e.g. dancing). Previously, bacha bazi was included in anti-trafficking legislation, with illegal acts associated with it such as sexual violence covered under the previous penal code; however, the revised penal code brought together provisions related to the criminalisation of bacha bazi into one law, clarifying and confirming the elements of the crime and associated sanctions. According to these provisions, perpetrators of bacha bazi may face up to seven years of imprisonment, those keeping multiple boys under the age of 12 may face life imprisonment, and members of the Afghan national security forces involved in bacha bazi may face up to 15 years of imprisonment. Further, the penal code criminalises those participating in events where bachas dance or perform.[37]
In March 2019, the Child Rights Protection Law (Child Act) was enacted by the President through a Legislative Decree (No. 362). Chapter 15 includes provisions for the protection of children against prostitution, sexual activities and sexual exploitation and abuse, including Article 96 which prohibits the “persuasion or coercion of a child to engage in every kind of sexual activity or usage in prostitution or other illegal sexual activities or/and in pornographic images and videos.”[38] Article 99 prohibits bacha bazi, stating that “Bacha Bazi is a crime, any person committing it, privately or publicly, individually, or collectively, shall be punished in accordance with the provisions of law.”[39] Attempts to pass the law through Parliament have not been successful, with the Wolesi Jirga (lower house) continuing to debate the Child Act based on the legal definition of a child.
Despite challenges to passing the Child Act through parliament, children’s rights organisations are hopeful that the revised Penal Code and the Child Act will help to fight against impunity of perpetrators. However, the criminalisation of bacha bazi in the 2018 revised Penal Code and prohibitions in the Child Act do not appear to have led to increased accountability for the perpetrators of these crimes, with little indication that the practice of bacha bazi has reduced or that those responsible are prosecuted or convicted for their crimes.[40]
Legal frameworks that address sexual violence against adult men are less clearly articulated. In the previous iteration of the Penal Code, article 429 stated that: “A person who, through violence, threat, or deceit, violates the chastity of another (whether male or female), or initiates the act, shall be sentenced to long imprisonment, not exceeding seven years.”[41] Under the revised Penal Code, rape against any person, including male or female, is more clearly articulated, with perpetrators subject to long imprisonment (Article 637) or, in cases of gang rape, the death penalty or grade one continued imprisonment from 20 to 30 years (Article 641). Article 636 of the revised Penal Code defines rape in the following way:
“A person who has sexual intercourse with another person or penetrates body parts or any other object in vagina or anus of the victim using the following means: force, threat, other intimidating means; taking advantage of physical or mental disability of victim, or disability of the victim to express consent, including male or female, or by feeding sedative drugs or other substances that alters state of consciousness shall be deemed perpetrator of rape.”[42]
Despite this definition of rape including both males and females, there are a number of additional provisions in the Penal Code that complicate protection for men. The revised Penal Code states that in cases where a person “commits aggression to chastity and honour and dignity of a female” without anal or vaginal penetration, they will be sentenced to up to seven years imprisonment (Article 640), essentially omitting coverage of males from forms of sexual violence that do not include rape. Further, legal provisions proscribing rape of males under the Penal Code are complicated by other provisions that de facto prohibit same-sex sexual acts, including sodomy, and tafkhez and mosahiqah (sexual acts that do not result in penetration).[43] The findings in research conducted by UN actors and NGOs that boys who have been the victims of rape may be incarcerated for pederasty or other moral crimes suggest that the legal lines drawn between consensual and non-consensual sex are often blurred.[44] This blurring may also impact on adult men, although it is unknown if, or the extent to which, men are prosecuted for having same-sex relationships when they have in fact been raped.
The Role of Communities in Supporting Male Victims/Survivors of Sexual Violence
Before analysing in more detail the availability and quality of healthcare services for male victims/survivors of sexual violence in static healthcare facilities, it is helpful to examine the possible role that communities might have in supporting male victims/survivors, and some of the barriers they may face in doing so. When research participants were asked to reflect on the role of communities in supporting male victims/survivors of sexual violence, particularly their access to healthcare facilities, their reflections were largely framed around the roles of CHWs and community leaders.
Community Health Workers
As outlined in the introduction to this report, CHWs are part of the MoPH’s BPHS and comprise volunteers who support villages in their catchment area with basic healthcare services and referrals to healthcare facilities. Only one male CHW interviewed for the research reported having provided assistance to a male victim/survivor of sexual violence. The remaining CHWs stated either that there had not been any such cases in their community catchment areas, or that there had and that CHWs had not played a role in supporting the male victim/survivor.
Overall, CHWs, healthcare providers and male victims/survivors agreed that CHWs had played, or could play, an important role in referring male victims/survivors of sexual violence to healthcare facilities and, in some cases, providing very basic healthcare support such as first aid (e.g., bandaging of superficial wounds) and provision of analgesics for pain. Some CHWs suggested that they could also provide basic psychosocial support and counselling to male victims/survivors if required; however, most CHWs and healthcare providers emphasized that CHWs did not have the capacity to provide this kind of support and that their main role was as an entry point to formal health facilities through referrals. The relationship between CHWs and healthcare providers is reciprocal insofar as CHWs also appear to serve as bridges between healthcare providers and communities in cases where healthcare providers need to communicate with community members, including to raise awareness about available services.
In describing how they would support male victims/survivors of sexual violence if faced with such a situation, CHWs had conflicting perspectives about how this would be done in a way that respected victim/survivors’ rights to privacy, confidentiality and consent. All CHWs interviewed for the research stressed the importance of confidentiality if a victim/survivor asked them for assistance and some CHWs could clearly describe how confidentiality would be ensured; for instance, by speaking with victims/survivors in a private space, asking for their consent to report the case to families or services (e.g., healthcare services or the police), not reporting the case if consent was not provided and, if sharing information about the case with healthcare providers to seek advice, only doing so without naming or identifying the individual. However, a quarter of CHWs interviewed for the research gave examples of hypothetical cases in which they would breach the confidentiality of a male victim/survivor, in most cases without realising that this would be a breach. Several CHWs reported that they would share the case with the victim/survivor’s family member or community leader, in the latter case under the assumption that it was their responsibility to ensure confidentiality, and several suggested that they would report the case to a healthcare provider with or without the consent of the victim/survivor.
CHWs’ inconsistent reports of how they would ensure the confidentiality of male victims/survivors may be linked to broader gaps in their capacity in relation to supporting victims/survivors of violence, whether male or female. Five CHWs interviewed for the research reported having participated in training on GBV, four of whom are from Balkh province. When asked about the content of GBV training, two CHWs stated that the training only covered violence against women, two stated that the training covered topics related to both male and female victims/survivors of violence and one stated that the training covered sexual violence against children, albeit without reference to whether this included girls and boys. When asked about what training or support could assist them to improve health services for male victims/survivors, CHWs showed strong interest in participating in corresponding training and workshops. Particular topics of interest included how to raise awareness about sexual violence against men and boys at the community level, how to provide mental health and psychosocial support to male victims/survivors and how to encourage them to access healthcare services in cases where they are reluctant to do so.
Community Leaders
Traditional and religious leaders at the community level were identified as both important actors in facilitating support for male victims/survivors of sexual violence and, conversely, key actors reproducing stigma and violence against male victims/survivors to punish them for the violence they had experienced.
Male victims/survivors, healthcare providers and CHWs positioned community-level traditional elders and religious leaders as fulfilling a number of possible functions in the support of male victims/survivors. A key perceived function was in awareness-raising of the rights of all victims/survivors, including men, women, boys and girls, to live free of violence. Religious leaders are perceived to be particularly important actors in this regard and a number of research participants noted how they could disseminate messaging about violence prevention and the prevention of stigma and blame of victims/survivors through Friday prayers in mosques and through their daily communication with families and community members. In contrast, traditional leaders including elders and maliks (village heads) are positioned as more important actors in supporting response rather than prevention by supporting victims/survivors to access services, including health and legal services. In relation to health services, several CHWs and healthcare providers in Balkh and Kandahar mentioned that elders and community leaders formed part of community health councils that coordinate with local healthcare facilities, and that these councils could play an important role in raising awareness about sexual violence against men and boys and supporting victims/survivors to access healthcare facilities. One stakeholder interviewed for the research, from an NGO implementing the BPHS in Kandahar, also noted the importance of community health councils in acting as a bridge between healthcare facilities and communities.
Despite widespread perceptions that traditional and religious leaders could play an important function in raising awareness about male victim/survivors’ rights to live free from violence and how to access formal services, more than three quarters of research participants stated that this is not currently happening. One area in which traditional leaders were described as active was in informal dispute resolution. A number of victims/survivors, healthcare providers and CHWs, in Kandahar in particular, suggested that traditional leaders played an important role in resolving disputes between victims/survivors of violence and perpetrators through traditional mechanisms (shura or jirga). In noting this role of leaders in informal dispute resolution, few research participants acknowledged that sexual violence was a crime that should be addressed by the formal justice system. However, the issue of corruption in the formal justice system was raised as a key reason that victims/survivors and their families may prefer to use informal dispute resolution mechanisms led by elders and traditional leaders. Despite concerns about corruption in the formal justice system, several research participants noted that traditional leaders were not immune from corruption and that informal dispute resolution processes may work in favour of the perpetrator if he was wealthy and able to bribe the shura or jirga. In some cases, traditional leaders or people within their family or social networks may also be perpetrators of sexual violence against men and boys. Several CHWs also noted that if the perpetrator was powerful and armed, traditional and religious leaders would be powerless to seek informal justice on behalf of victims/survivors.
Regardless of perceptions of the usefulness of traditional and religious leaders in raising awareness about the rights of male victims/survivors or informally resolving their cases, more than half of the male victims/ survivors interviewed for the research stated that traditional and community leaders were to be feared as perpetrators of emotional and physical abuse. Some victims/survivors reported fearing that community leaders would verbally abuse them and eject them from the community, while others reported fearing that they would be killed by religious leaders if their case of sexual violence was disclosed to the community due to same-sex sexual activity or transgender identity being perceived as un-Islamic and punishable by death. As one male victim/survivor from Kabul stated of religious and community leaders, “From the perspective of Sharia law, they consider this incident illegal and prohibited, so they may threaten him with death by stoning.”
Healthcare Services for Male Victims/Survivors of Sexual Violence
This section of the report describes in more detail the perspectives of male victims/survivors and healthcare providers on the care pathway for male victims/survivors in health facilities, and the typical experiences that men and boys might expect to have in receiving care, including survivor-centred care. It should be noted at the outset that only 11 victims/survivors reported ever having accessed healthcare facilities for the sexual violence they experienced, and four of these had only accessed YHDO health services, which were reported to provide psychosocial counselling and testing for HIV and other sexually transmitted infections (STIs), alongside other services such as justice and livelihoods support. Further, only nine healthcare providers reported having provided healthcare support to a male victim/survivor of sexual violence. Consequently, the perspectives shared in the research were hypothetical for many participants. This was expected given the research team’s understanding of the healthcare sector being a rarely used entry point for male victims/ survivors of sexual violence. Nevertheless, victims/survivors’ narratives about what they think would happen at a healthcare facility provide a useful entry point to understanding their concerns about the care they expect to receive. Similarly, although few healthcare providers had direct experience providing services to male victims/survivors, their descriptions of what the care pathway would be should a victim/survivor attend their healthcare facility provide important information about both the strengths and gaps in healthcare provider knowledge and attitudes and the protocols in place in healthcare facilities to support male victims/ survivors of sexual violence.
Steps in the Care Pathway
In describing the different steps in the care pathway, this sub-section of the report does not attempt to replace the formal flow charts guiding care in different types of health facilities but, rather, attempts to document the typical steps in healthcare pathways that male victims/survivors in particular might expect to take. As expected, the healthcare pathway for male victims/survivors described by healthcare providers differs according to the type of health facility, with fewer steps in the care pathway in smaller facilities such as BHCs and CHCs, and more steps in the pathway in larger facilities, including district and provincial hospitals.
When asked about the types of staff members in a health facility that a male victim/survivor would likely come in contact with, approximately half of healthcare providers and just over half of victims/survivors mentioned the security staff at the entry of the health facility as the first point of contact. According to healthcare providers, although security staff have the primary role of guarding the facility and conducting pat down search checks on patients, they often have additional roles. These include showing patients how to access the reception desk or, in the case of smaller facilities such as BHCs and CHCs that may not have a reception desk, providing patients with numbers to wait in a queue to see a healthcare provider. One healthcare provider from a BHC in Balkh suggested that guards may also participate in triage by determining the severity of a patient’s case. However, overall, healthcare providers suggested that security staff have little verbal contact with victims/survivors and would not obtain any information from them about the reason they wanted to see a healthcare provider.
For those healthcare facilities with a reception or administration desk, this is the next step in the care pathway for male victims/survivors. Healthcare providers suggested that reception or administration staff are primarily responsible for recording patient information and directing them to the appropriate section of the facility. Although the majority of healthcare providers stated that this would occur by asking the patient for general information about which type of healthcare service he required, several providers suggested that reception staff may ask them explicitly about their case in order to direct them to the appropriate healthcare provider. It is interesting to note that this more explicit request for information about an individual’s case was only described in larger health facilities, including private and provincial hospitals.
According to healthcare providers, the next steps in the healthcare pathway depend on the type of facility and the type of service requested or needed by the victim/survivor. In smaller health facilities such as BHCs and CHCs, healthcare providers suggested that a male victim/survivor would be directed to see a doctor in the outpatient department (OPD) and, if the victim/survivor had serious injuries, be referred to the emergency room (ER) of a district or provincial hospital. Healthcare providers in district, provincial, regional and private hospitals suggested that in cases where male victims/survivors had no visible injuries, they would be directed to a doctor in the OPD where they would have a medical consultation. Based on the outcome of the consultation, victims/survivors may be directed to the laboratory for blood or other tests or to a pharmacy if medication is prescribed. In cases where victims/survivors have injuries, they would receive first aid or treatment in the OPD, sometimes by a nurse in cases of minor injuries (e.g., minor dressing of wounds), or by a medical specialist in the ER in cases of serious injuries where they may require surgery (e.g., in the case of severe anal injuries). According to most healthcare providers, regardless of the type of facility, after receiving treatment male victims/survivors would be referred to psychosocial counselling services, either externally for smaller facilities or internally for larger facilities.
Several healthcare providers also mentioned the importance of referring victims/survivors to the medical forensic section of a health facility to undergo further tests and to judiciary services, including the police; however, in both cases, healthcare providers emphasized that this would only occur with the consent of the victim/survivor or in the case of children with the consent of a parent or caregiver.[45] Those healthcare providers who mentioned forensic medicine noted that this service was not available in smaller health facilities and victims/survivors would need to be referred to a provincial or regional hospital to undergo medical forensic tests and documentation or to receive medical forensic care. One healthcare provider in a regional hospital noted that even where forensic medicine was available, there were limitations in what forensic medical healthcare providers could do for victims/survivors given lack of equipment and diagnostic capabilities.
Survivor-Centred Care
Healthcare providers and victims/survivors were asked to describe whether and how survivor-centred care would be provided to male victims/survivors of sexual violence within healthcare facilities. This was not asked directly but rather through a series of probes around the care pathway, including about how healthcare providers would treat male victims/survivors, ensure confidentiality and privacy, victim/survivor feelings of choice and control and, for healthcare providers, what kinds of protocols were in place at the facility level to support this care. As noted previously, few healthcare providers had ever provided care to men or boys who had experienced sexual violence and descriptions of survivor-centred care and protocols for men and boys appear to be explicitly derived from established procedures for women and girls (where these exist). For ease of reference, where relevant, the findings outline how these procedures are defined by the GBV Treatment Protocol for Healthcare Providers in Afghanistan in order to identify the extent to which current practices and systems to address the needs of male victims/survivors are aligned with the Protocol.
Respect, Empathy and Non-Judgement
When asked how they would treat male victims/survivors of sexual violence attending their healthcare facility, the majority of healthcare providers interviewed stressed that all victims/survivors would be treated well, with respect and empathy, and that they would not be blamed or judged for the violence they have experienced. Only four healthcare providers suggested that although this was how it should be, not all healthcare providers behaved in this way. One male healthcare provider working in mental health in Balkh province noted that despite the mental health section of the facility working on removing stigma towards victims/survivors, staff members with less experience and training might be less successful in doing so, leading to victim/survivors’ mistrust in healthcare providers. Other healthcare providers who suggested that staff behaviour towards male victims/survivors may be negative also emphasized lack of training.
The issue of judgement and blame was a reoccurring theme, and healthcare providers in general highlighted the importance of not blaming victims/survivors for the violence they had experienced. However, some healthcare providers did reproduce blame in a more indirect way by suggesting that part of the healthcare treatment would involve advising victims/survivors “not to do it again”, which assumes that the victim/survivor had a choice and could continue to choose not to be raped. Some healthcare providers made more direct references to male victims/survivors participating in sex work, and healthcare providers’ roles in advising them to “stop doing these bad things” or “leaving this profession”. Despite these few isolated cases, healthcare providers’ descriptions of respect, empathy and non-judgement towards male victims/survivors are broadly in line with the guidance presented in the GBV Treatment Protocol (see Box 3).
There was some dissonance between how healthcare providers described the way they would behave with male victims/survivors of sexual violence and the kind of treatment from healthcare providers that male victims/survivors have experienced or believe they will experience in a healthcare facility. The majority of victims/survivors interviewed recognised that the quality of treatment would likely vary across different healthcare providers and that some may treat victims/survivors well and others poorly. Much like healthcare providers, male victims/survivors stressed that not being judged or blamed was one of the most important behaviours they would want from a healthcare provider. However, many of the victims/survivors interviewed for the research did not feel confident that this is the behaviour they would experience if they did access a health facility. As outlined in the section of this report on stigma from healthcare providers as a barrier to access to healthcare, male victims/survivors are fearful of being mistreated and humiliated by healthcare providers and this fear is particularly pronounced for victims/survivors with diverse SOGIESC.
The GBV Treatment Protocol articulates guidance on ensuring respect, empathy and non-judgement for all survivors, whether male or female (see Box 3). The guidance emphasizes the importance of adopting a respectful attitude, not judging the survivor, guaranteeing confidentiality, being empathetic and showing patience. However, the section on survivor-centred care does not differentiate between female and male survivors, or whether typical healthcare provider attitudes about survivors, including stigmatising attitudes, might be different based on the gender of the survivor. Further, there is no specific guidance for different types of male survivors who may be at greatest risk of experiencing stigmatising attitudes and behaviours, such as those with diverse SOGIESC or those who are engaged in sex work. It is recognised that this is likely due to diversity in sexual orientation and gender identity being an extremely sensitive topic in Afghanistan, and homosexuality being criminalised under the Penal Code. However, there is a substantial gap in understanding how healthcare providers can be supported to provide non-stigmatising treatment to all male victims/survivors, regardless of their identities or characteristics.
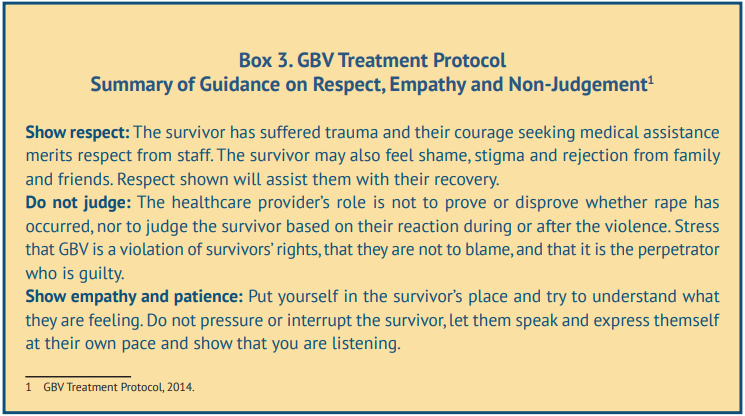
Privacy
All healthcare providers recognised the importance of victim/survivors’ privacy and that a consultation should take place in a private room separated from other patients, in line with the guidance provided in the GBV Treatment Protocol (see Box 4). Several healthcare providers noted that facilities have separate male and female OPDs where private consultations could take place. Although most healthcare providers stated that privacy for victims/survivors was standard procedure and always respected, there appear to be some challenges to maintaining privacy in different types of facilities. In smaller healthcare facilities, such as BHCs and CHCs, healthcare providers may face more challenges in finding adequate space to separate patients, and one CHC healthcare provider noted that there were no specific spaces to treat GBV victims/ survivors in their facility. One healthcare provider in a regional hospital also suggested that privacy for victims/survivors might be difficult to ensure due to the very large number of patients and subsequent crowding, despite the larger size of the regional facility. No healthcare providers referred to ensuring privacy by managing patient flow and reducing requirements for victims/survivors to move throughout multiple spaces in the care pathway. One male victim/survivor in Kabul who had received healthcare services in the past noted his dissatisfaction with being asked about the violence he experienced while there were many other healthcare providers present, highlighting the importance of minimising patient flow and ensuring others, including other healthcare providers, are not present when asking about GBV.
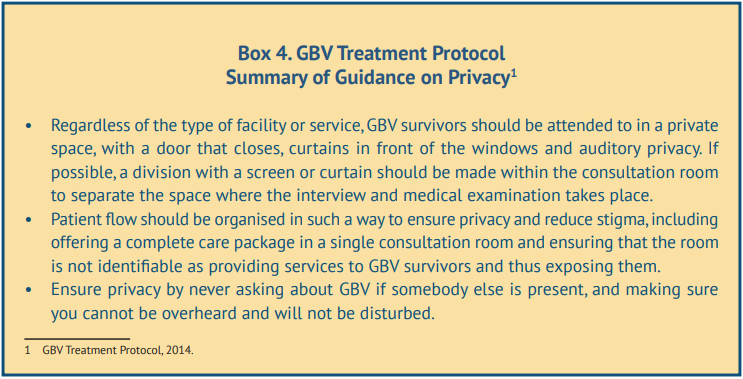
Confidentiality in Healthcare Facilities
All healthcare providers interviewed stressed the importance of confidentiality and that this was a fundamental principle applied to the treatment of all patients, particularly victims/survivors of violence. Healthcare providers described a number of procedures they would implement to ensure the confidentiality of a male victim/survivor of sexual violence attending their healthcare facility, mainly in relation to providing services in a private setting. Healthcare providers also made reference to information management procedures that are in line with the guidance provided in the GBV Treatment Protocol, including managing referrals and sharing of patient information in a confidential manner (see Box 5).
In relation to managing referrals and sharing patient information within the same healthcare facility, the procedure reported by healthcare providers was to only refer victims/survivors to other services with the patient’s consent. Despite broad agreement with this procedure in principle, there was some variation in how healthcare providers described providing referrals internally within the same facility. This variation appears to be partly related to the type of facility. In smaller facilities, healthcare providers were more likely to report making internal referrals to other healthcare providers and sharing victim/survivors’ case details with them only with the consent of the victim/survivor. In contrast, several healthcare providers in larger facilities were less clear about the process of maintaining confidentiality and obtaining consent when making internal referrals and sharing case details across different facility providers and departments. For instance, one healthcare provider in a regional hospital noted that given the multiple points in the care pathway, confidentiality is more likely to be violated as the number of healthcare providers involved with the case increases. The assumption in this example is that victims/survivors are not necessarily asked for consent for their information to be shared with all healthcare providers from whom they receive services in the care pathway.
There was more consistency in healthcare providers’ descriptions of victim/survivor confidentiality and consent to share information when making referrals to external services and organisations. Healthcare providers emphasized that victims/survivors were required to consent to having case information shared with external health facilities to which they were being referred, whether within or outside of the BPHS structure. Healthcare providers also referred to de-identifying victim/survivors’ data if sharing details of their case outside of the healthcare facility, such as with NGOs supporting case management.
There was some variation in victim/survivors’ perspectives on the extent to which healthcare providers would respect their confidentiality. As outlined previously in this report, when asked about the barriers to access to healthcare facilities, fears emerged of healthcare providers breaching confidentiality and disclosing victim/ survivors’ cases to families and community members. Nevertheless, victims/survivors generally recognised that it was the responsibility of healthcare providers to ensure the confidentiality of their disclosure of violence. Most victims/survivors interviewed for the research had some level of confidence that healthcare providers would maintain their responsibility to respect confidentiality, although this was perceived to depend partly on the quality of the provider. There were three situations in which victims/survivors thought a healthcare provider might breach confidentiality, including: if the healthcare provider knew the victim/survivor personally or lived in or near the same community; if the healthcare provider stigmatised or disrespected the victim/ survivor, or treated him as guilty; or if the healthcare provider felt compelled to report the case to legal and judicial actors without the consent of the victim/survivor. In relation to this latter point, given victim/ survivors’ fears of cases being reported to judicial actors without their consent, and this fear constituting a significant barrier to their access to healthcare facilities, a discussion of confidentiality and referrals to judicial actors is included separately in the following section.
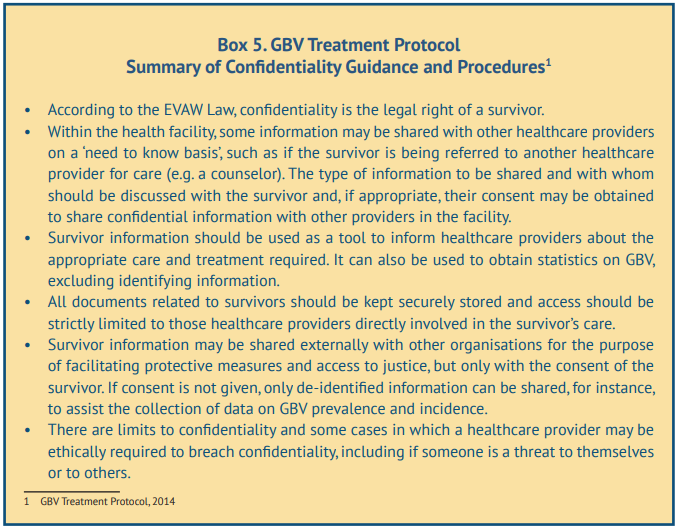
Confidentiality and Referrals to Judicial Actors
As outlined previously in this report, when asked about the barriers to male victim/survivors’ access to healthcare facilities, fears emerged of healthcare providers breaching confidentiality and disclosing cases to judicial actors. In large part, victim/survivors’ fears do not appear to be aligned with the practices reported by healthcare providers. In relation to referrals to justice and legal services, most healthcare providers emphasised that they would not refer a victim/survivor’s case to judicial actors without victim/survivor consent. In cases where victims/survivors do not consent to have their case reported to the justice or legal sector, healthcare providers described being required to report cases to the police but without any personal or identifying details of the victim/survivor. This is largely in line with the confidentiality procedures presented in the GBV Treatment Protocol, which highlight that de-identified data can be shared with outside organisations for the purpose of compiling data on GBV prevalence (see Box 5).
Despite broad agreement among healthcare providers that male victim/survivors’ cases would not be reported to judicial or other actors (with identifying information) unless victims/survivors consented and wanted to seek legal and judicial support, there were some exceptions, particularly in Balkh province. Two male healthcare providers in Balkh, one in a district hospital and another in a regional hospital, stated that cases involving sodomy were classed as criminal and that healthcare providers were required to report these cases to the criminal department, or to forensic medical services in other facilities, with or without the consent of the victim/survivor. Another male healthcare provider in a regional hospital in Balkh stated that although they tried to maintain confidentiality of male victims/survivors, there were cases in which they had to breach confidentiality and share case details with the police or the criminal department, although he did not state whether this would be done with the victim/survivor’s consent or not. One healthcare provider in a private hospital in Balkh also noted that cases involving sodomy or MSM were classed as criminal and had to be referred to forensic medical services in a public hospital given that private facilities are not legally able to provide forensic medicine or refer victims/survivors to judicial services. He did not state whether this would occur with the consent of the victim/survivor, although healthcare providers in private facilities in other provinces stated that this process would only occur consensually.
It is unclear from the above examples in Balkh the extent to which healthcare provider reports to judicial actors, including when breaching confidentiality, are in line with legal requirements. There are some gaps in the GBV Treatment Protocol in relation to whether male survivors of sexual violence should be treated according to the same or a different legal framework than women and girls. The Protocol’s section on legal framework and rights of survivors draws specifically from the EVAW Law and refers only to women, and stipulates that female survivors have the choice to instigate the criminal justice process or not, and that mandatory reporting of GBV cases is not required (see Box 6). Given that men and boys are not covered by the EVAW Law, it is unclear the extent to which these regulations within a health facility should be followed also for male victims/survivors, or whether gaps in the Penal Code addressing sexual violence against men (in particular) may put male victims/survivors at risk of confidentiality breaches from healthcare providers.
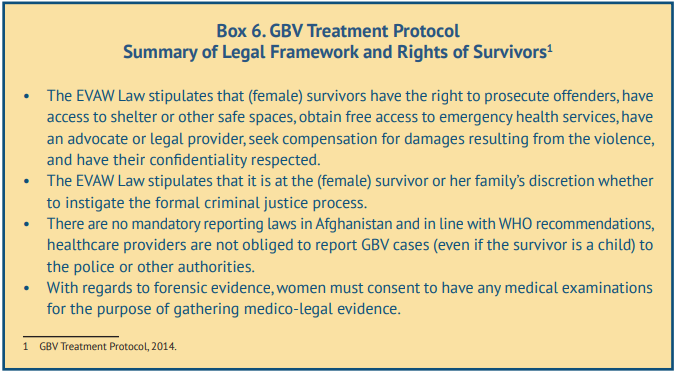
Safety
Male victims/survivors were asked about how safe they would feel accessing healthcare services to receive treatment due to sexual violence they had experienced. Almost all victims/survivors associated feelings of safety with assurances that their case would be treated confidentially and not disclosed to others. However, as outlined in the section of this report on threats of further violence as a barrier to seeking healthcare, a small number of victims/survivors reported fears for their physical safety if they accessed a healthcare facility, particularly the risk of being raped by a male healthcare provider.
These fears appear to be more pronounced if male victims/survivors have diverse SOGIESC. Victims/survivors also referred to fears of other types of mistreatment or abuse if healthcare providers identified them as having a diverse SOGIESC. For instance, one victim/survivor described fear of being touched inappropriately by a healthcare provider who may want to examine his genitals out of curiosity about his gender identity, while another victim/survivor suggested that healthcare providers might try to establish intimate, albeit consensual, relationships with victims/survivors.
Choice and Control
Male victims/survivors were asked about the extent to which victims/survivors would have choice and control in decision-making about their own healthcare when accessing a health facility. Almost all victims/survivors interviewed said that they expected that they would have some level of control over the healthcare options presented to them and could not be forced to accept a recommendation from a healthcare provider. However, most victims/survivors also suggested that the ultimate choice and authority should lay with the healthcare provider, who was best positioned to know what victim/survivors’ needs were and how to address them.
When asked how a healthcare provider might react if a victim/survivor rejected the recommended treatment, victims/survivors described two different types of reaction. One was anger and possibly the ejection of the victim/survivor from the facility, which some victims/survivors perceived to be appropriate given their beliefs that healthcare providers were knowledgeable about victim/survivors’ needs and should have authority in the decision-making process. However, victims/survivors more commonly described welcoming a fluid process of negotiating choice whereby a good healthcare provider would try to persuade the patient to adopt the recommended treatment by providing more information about possible choices, speaking in a respectful and kind manner or giving the victim/survivor time and space to consider his options before making a decision. Several victims/survivors suggested that this positive behaviour would help to build their trust in the recommendations of healthcare providers. Only two victims/survivors suggested that male victims/ survivors should not have a choice and that healthcare providers should proceed to treat the patient with or without his consent.
Healthcare providers’ descriptions of how they facilitate victim/survivors’ choice and control over treatment and services are largely in line with the negotiation process outlined above, and are also in line with the guidance on survivor empowerment, choice and control outlined in the GBV Treatment Protocol (see Box 7). When healthcare providers referred to the process of supporting choice and control, they explained that they would provide information about the treatment and care possibilities, including additional services to which to refer victims/survivors, and that a decision to move forward with any plan would only be made in agreement with the patient. However, much like victims/survivors, healthcare providers emphasized that they were knowledgeable about the requirements of patients and that part of their job was to convince victims/survivors to follow an appropriate treatment and referral plan through provision of information and support rather than coercion. Several healthcare providers noted that victim/survivors’ decisions not to adopt a recommendation for treatment or referral were not always due to their disagreement with the proposed options, but may be due to financial barriers that restricted their ability to pay for certain treatments or services.
Specific Considerations for Children
As outlined in the methodology section of this report, the research did not sample male victims/survivors under the age of 18 years, leaving a gap in the research given that the perspectives of boys were not captured directly. However, several male victims/survivors disclosed that they had first experienced sexual violence as a child. Healthcare providers also described how services may differ for boys in comparison with adult men, and several healthcare providers reported having previously provided services to boy victims/survivors of sexual violence. Consequently, some retrospective analysis of healthcare provision for boys is possible. Given international recognition of the evolving capacities of the child, and the GBV Treatment Protocol’s specific considerations for children (see Box 8), the analysis of healthcare provision and survivor-centred care for boy victims/survivors of sexual violence is presented separately.
According to WHO guidance for the health sector’s response to children and adolescents who have been sexually abused, the principle of evolving capacities of the child refers to the capacity of children and adolescents to understand information about healthcare, including its benefits and consequences, and to make informed choices about care, evolving according to a child’s age or developmental stage. This requires healthcare providers to: provide information that is appropriate to a child’s age and other intersecting characteristics (e.g. sex, race, ethnicity, religion, SOGIESC, disability); seek consent and assent as appropriate, recognising that it may sometimes be in the best interest of a child or adolescent to waiver caregiver consent (including if the caregiver may be a perpetrator of violence, or if the child might be placed at further risk through disclosure to a caregiver); respect the autonomy and wishes of children and adolescents while balancing this with the need to protect their interests; and offer choices in the course of their healthcare.[46] The Afghanistan GBV Treatment Protocol outlines a number of specific considerations for children survivors of violence that are in line with the principle of evolving capacities of the child (see Box 8).
Healthcare providers were asked to describe how the care pathway and their provision of services might differ between adult and child male victims/survivors of sexual violence. Notably, 40% of healthcare providers stated that there was no difference in how an adult or child would be treated.
Of the 60% of healthcare providers who did state that provision of care would differ between boys and adult men, most described the key difference as requirements for the intervention of caregivers in the case of minors. Half of these healthcare providers suggested that children were unable to understand the information provided and that healthcare providers would rely on caregivers to accompany the child and communicate and make decisions on behalf of the child. One fifth of healthcare providers who acknowledged different provision of care between children and adults emphasized that parental consent was mandatory when making healthcare decisions for children and adolescents. One healthcare provider stated that in cases in which a child victim/survivor of sexual violence approached a healthcare facility alone, the facility staff may also need to break their confidentiality in order to locate the child’s family members if the child is unable to provide a contact or address, despite this being potentially harmful to the child.
Among the healthcare providers described above, there appeared to be little recognition that the ability of children to communicate about their situation or care, or be asked for consent or assent to receive healthcare services, may depend on their age and developmental capacities. Two healthcare providers, both of whom had provided care to boy victims/survivors of sexual violence in the past, did state how they had age-appropriately communicated with and provided treatment for boys, although in both cases they reported having broken the confidentiality of the child. For instance, according to one healthcare provider in Kandahar:
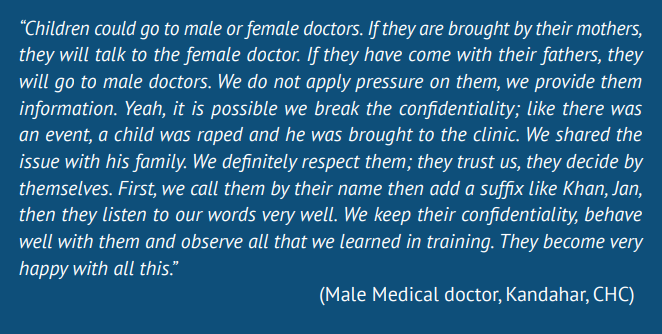
The second healthcare provider, a female CHC clinic manager in Kabul, also reported having provided services for a boy victim/survivor of sexual violence. She described at length the process of holding a consultation with the boy in private, examining him, building trust and ensuring that the boy agreed to different steps in the care pathway. However, the healthcare provider disclosed the outcome of the medical examination and consultation with the boy’s mother, despite the boy requesting her not to do so, and then requested the mother to keep the disclosure a secret (see Box 9).
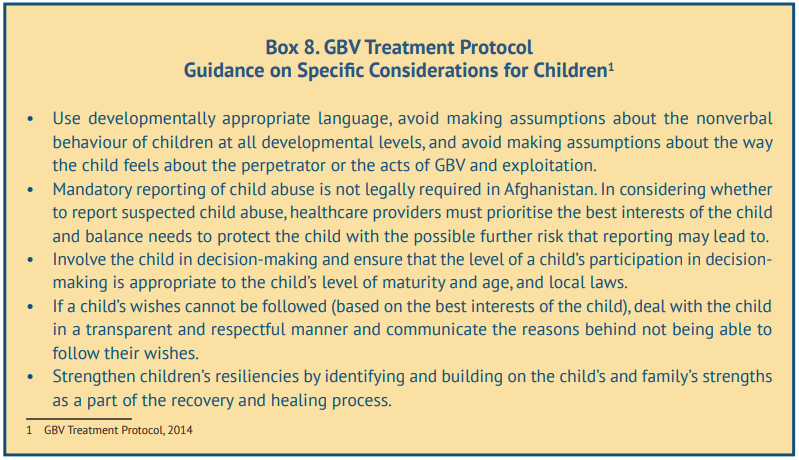
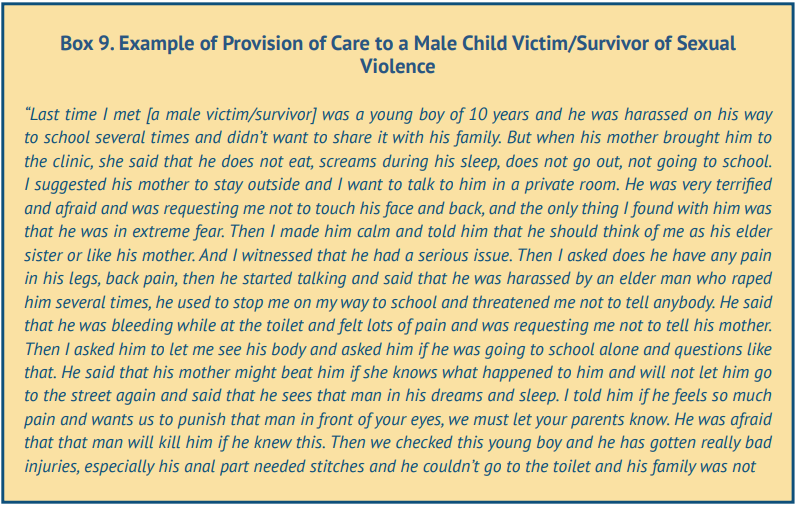
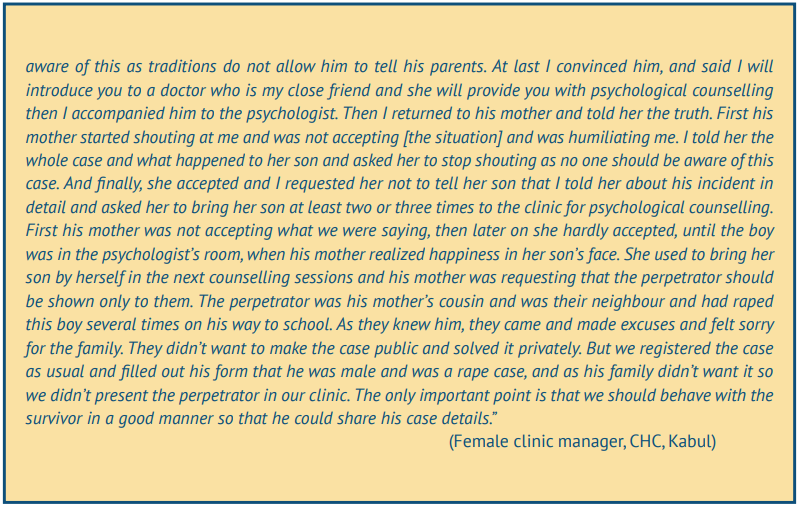
Needs of Male Victims/Survivors of Sexual Violence
Research participants were asked to reflect on the needs of male victims/survivors of sexual violence, including their healthcare needs and other needs they may have, and how healthcare providers could support them to address these needs. This section summarises these needs, with a focus on analysing where there is agreement or difference between victim/survivors’ self-identified needs and the needs of men and boys perceived by healthcare providers, and any resulting gaps in the ability of healthcare providers to deliver quality services to male victims/survivors of sexual violence.
Healthcare Needs
Male victims/survivors made general references to requiring access to healthcare services if they experienced sexual violence, and also made more specific references to the kinds of services they would expect such as treatment of injuries and wounds, testing for STIs including HIV, and access to medicines. Victims/survivors also emphasized their need for psychosocial counselling and support and described the severe psychological impacts of experiencing sexual violence, including depression, anxiety, social isolation and suicidal thoughts or suicide attempts.
Healthcare providers also highlighted male victim/survivors’ needs for treatment of their physical injuries and psychosocial support. Although they felt equipped to provide treatment for injuries, the majority of healthcare providers interviewed suggested that facilities, even large facilities such as provincial and regional hospitals, had insufficient psychosocial services for victims/survivors of sexual violence and that this was a particular gap that needed to be addressed. One stakeholder in the health sector stressed that the gap in availability of psychosocial services was even greater for male victims/survivors of sexual violence and that existing psychosocial service providers did not currently have the capacity to deliver these services.
When asked about their needs, although victims/survivors noted specific services such as those outlined above, they more commonly emphasized the manner in which these services were delivered by healthcare providers. In particular, they highlighted the need for healthcare providers to respect their privacy and confidentiality, and to be treated with kindness and with no judgement, blame or stigma. Several victims/ survivors also stressed the need for healthcare providers to avoid treating men and boys with diverse SOGIESC in a negative and judgemental way, including staring at, teasing or humiliating them.
When healthcare providers were asked about the needs of male victims/survivors and what they most valued in a healthcare provider, the most common responses related to maintaining privacy and confidentiality, and treating victims/survivors with respect, dignity and without blame. This suggests that male victim/survivors’ and healthcare providers’ perceptions about the importance of the manner in which healthcare services are delivered are aligned. However, it is important to note that healthcare providers did not explicitly mention the needs of male victims/survivors with diverse SOGIESC or recognise them as a distinct vulnerable group requiring services. This may be due to the methodology employed in the research, which did not explicitly ask about victims/survivors with diverse SOGIESC. However, when prompted to discuss which men and boys were at greater risk of being victimised and how healthcare services should address their needs, healthcare providers did not refer to male victims/survivors with diverse SOGIESC.
This may suggest that there is a gap in understanding of the risks facing this particular group, or that some healthcare providers do not classify men and boys with diverse SOGIESC as victims/survivors of sexual violence. Two male healthcare providers in Balkh province stated that sexual intercourse between men was wrong, and one stated that it was anti-Islamic and would incur heavy punishment. One stakeholder interviewed for the research who works for a human rights organisation suggested that service providers, including healthcare providers, reproduce strong stigma towards adult male victims/survivors of sexual violence due to assumptions that they consented to the act as homosexual men and, thus, that the case would be classed as sodomy, which is illegal under the Afghan Penal Code. The finding in Balkh that three healthcare providers stated that they would report cases of sodomy to the criminal department, police or medical forensic services (two healthcare providers stating that they would do so without the consent of the male victim/survivor), may point towards some individuals’ experiences of sodomy being assumed to be consensual rather than rape.
Support From Family and Friends
One of the most important needs stated by male victims/survivors was the support of their family and friends. In particular, victims/survivors said that they needed their family and friends to support them by not judging or blaming them, and to encourage them to access healthcare or justice services and to accompany them when needed. Trusted friends appear to be a common source of information about healthcare services, particularly friends who know about the victim/survivor’s experience of sexual violence. A few victims/ survivors mentioned the exchange of information about services between friends who were from the same group, including victims/survivors with diverse SOGIESC or victims/survivors who had been sexually exploited through practices such as bacha bazi and who had developed social networks with other victims/survivors.
Healthcare providers also emphasized the importance of support from family and friends and, much like victims/survivors, suggested that family and friends could play an important role in encouraging them to access healthcare facilities. Healthcare provider perceptions of the importance of family and friends differed to those of victims/survivors in a number of ways that are consistent with healthcare provider beliefs about the causes of sexual violence against men and boys. They suggested that a key responsibility of family and friends was to regulate male victim/survivors’ social interactions to remove them from situations perceived to be risky and encourage victims/survivors to stop socialising with ‘bad’ groups. Healthcare providers also positioned family members as being important actors in providing children with sex and relationship education as a preventive measure.
Education and Livelihoods
Male victims/survivors frequently referred to dropping out of school as a key impact of their experience of sexual violence. A number of victims/survivors reported needing support to return to school and complete their education, or acquire vocational skills in order to pursue employment opportunities. Needs for educational access are further linked to needs for opportunities for livelihoods. Victims/survivors described their lack of education as a key barrier to obtaining adequate employment, locking them into poorly paid jobs that contributed to their and their families’ economic vulnerability. Several victims/survivors also referred to the dangers of being locked into sex work, which put them at increased risk of sexual violence. Healthcare providers also stressed the importance of supporting male victims/survivors to acquire education and obtain employment opportunities, but felt that this was largely an area that fell outside of their remit as healthcare providers. The one exception was where healthcare providers felt that they could counsel male victims/ survivors to stop engaging in sex work. Importantly, this was not a need identified by victims/survivors, who stressed that exiting sex work required having access to alternative livelihoods.
Justice
Almost all victims/survivors interviewed for the research stated that their needs after experiencing sexual violence included access to justice. Those victims/survivors who reported experiencing sexual violence for the first time at a young age, and who did not disclose the violence to a family member, noted that they lacked awareness of their rights to access legal services and justice for the violence they experienced. More generally, victims/survivors emphasized the need to ensure that perpetrators were prosecuted for the crime they committed to ensure they did not perpetrate sexual violence again. Healthcare providers also highlighted the importance of male victims/survivors seeking and obtaining justice, and perceived themselves as playing an important role in supporting this process by providing forensic medical services and referring victims/survivors to justice and legal services. As noted previously in this report, despite victim/survivors’ need for justice, they have strong fears of reporting cases in which perpetrators are armed or powerful actors. In these cases, healthcare providers are perceived to put victims/survivors more at risk of violence, including physical violence, if they refer cases to judicial actors. Further, although male victim/survivors’ fears of healthcare providers reporting their case to judicial actors without their consent appear to be largely misaligned with healthcare providers’ descriptions of confidentiality procedures, there may be some cases in which these fears are justified. A key gap in this regard may be the lack of clarity within formal protocols such as the GBV Treatment Protocol about the legal rights of male victims/survivors of sexual violence given they are not covered by the EVAW Law.
CONCLUSIONS
The results of this study suggest that the health sector is currently a vastly underused entry point for male victims/survivors of sexual violence in Afghanistan. This is due to multiple and cumulative barriers to male victim/survivors’ access to quality healthcare services.
Available anecdotal evidence suggests that feelings of stigma and embarrassment, and concerns about perceptions of their masculinity or sexuality, and that they were not able to prevent the assault, are key barriers to male victim/survivors’ access to healthcare facilities in Afghanistan. This research adds further weight to this evidence. It finds that the most significant barrier to male victims/survivors accessing healthcare facilities is fear of stigma and subsequent shame or loss of dignity, affecting both themselves and their families. Although male victims/survivors did not directly refer to stigma as a result of loss of masculinity, they did link stigma more directly to perceptions that they could not defend themselves or prevent the violence and were subsequently blamed for its occurrence. Stigma is perceived to be particularly pronounced for adult male victims/survivors given assumptions that they are more able to control, or defend themselves within, a situation of risk.
Male victims/survivors also feared stigma and negative attitudes from healthcare providers. Fears of being blamed or judged by healthcare providers appear to be particularly pronounced among male victims/ survivors with diverse SOGIESC. Healthcare providers rarely made any reference to male victims/survivors with diverse SOGIESC; however, they did appear to be aware of general fears that male victims/survivors had of the negative attitudes of healthcare providers, although most denied that these attitudes existed.
Concerns about stigma and shame feed into victim/survivors’ fears of disclosure of sexual violence to healthcare providers, and subsequent fears that they may be punished or experience further violence from perpetrators or even families if healthcare providers breach confidentiality and share their cases with others, including judicial actors. Victims/survivors also reported fears of being raped or sexually abused by healthcare providers, and suggested that male victims/survivors with diverse SOGIESC may be at particular risk. These fears of confidentiality breaches, or of experiencing further sexual violence at the hands of a healthcare provider, feed into deep lack of trust in healthcare provision, which restricts victims/survivors from accessing a healthcare facility or disclosing their experience of sexual violence to a healthcare provider.
Poverty is another key barrier to male victim/survivors’ access to healthcare facilities. Poverty and inability to pay for services, including fees in private facilities (which are often perceived to be of higher quality and safer) and for medications or other services in government facilities, were highlighted as important barriers. Further, victims/survivors with poor socio-economic status living in rural or remote areas were reported to struggle to pay for transport to access a healthcare facility at the district level or in the provincial centre.
Other barriers to access to healthcare services were linked to organisational limitations in healthcare provision. Although healthcare providers were able to articulate how survivor-centred care should be delivered to male victims/survivors of sexual violence, all healthcare providers interviewed for the research stated that their facility had no specific protocols for how to handle cases involving male victims/survivors or that they did not know if such protocols existed. Although the GBV Treatment Protocol for Healthcare Providers in Afghanistan does make some, albeit limited, reference to meeting the needs of male victims/survivors of sexual violence, few healthcare providers who were familiar with the Protocol or had been trained in its use remembered any content on men and boys. Further, healthcare providers and stakeholders recognised that there were large gaps in the availability of specialised services for male victims/survivors, with existing specialised services such as FPCs being targeted primarily towards women and girls. Healthcare providers and stakeholders welcomed additional training in how to meet the needs of male victims/survivors of sexual violence, and the development and implementation of centralised SOPs and protocols led by the MoPH and rolled out across the BPHS and EPHS.
The legal and policy environment in Afghanistan with regards to male victims/survivors of sexual violence appears to be an important structural barrier to help-seeking. Despite no legal requirements for mandatory reporting of GBV cases in Afghanistan, male victims/survivors reported strong fears that healthcare providers would disclose their case to judicial actors without their consent. These fears are likely linked to same-sex sexual acts being criminalised and concerns that, despite rape being criminalised under the Penal Code, healthcare providers will make judgements about whether sexual acts are consensual or non-consensual. The research found some examples, specifically in Balkh province, where this appears to be the case.
The research also identified several rape myths that circulate about why sexual violence against men and boys occurs. Male victims/survivors are more likely to reproduce victim-blaming discourses, perhaps due to internalised stigma and blame received from others. In contrast, healthcare providers are more likely to justify the behaviour of perpetrators by suggesting that social and cultural norms and practices, including expensive weddings and gender segregation, lead to men’s uncontrollable sexual desire. In either case, perpetrators are not portrayed as being actively responsible for the sexual violence they perpetrate, with the locus of responsibility being placed on victims/survivors and their families.
Communities may play an important role in reducing barriers to male victim/survivors’ access to healthcare facilities, but the resources they can direct towards supporting victims/survivors are currently being underused. Although CHWs do not play any formally recognised role in providing support to GBV victims/survivors and there has been some resistance to expanding their role to do so in Afghanistan, the research suggests that they could and sometimes do play a role in providing basic care to male victims/survivors and facilitating their access to static health facilities. They could also play a role in raising awareness about GBV, including sexual violence against men and boys. However, there are gaps in CHWs’ knowledge of how to provide confidential and survivor-centred care, likely due to lack of training and capacity-building opportunities.
Community leaders, religious leaders and members of community health councils may also play a role in reducing barriers to male victim/survivors’ access to healthcare facilities by raising awareness of sexual violence against men and boys and the prevention of stigma, and supporting victims/survivors to access services. However, in order for this to happen, significant work needs to be done with community leaders to raise awareness of the rights of men and boys who have experienced sexual violence to access formal justice and to shift leaders’ negative attitudes and potentially violent behaviours towards male victims/survivors.
The research attempted to understand the current practices of healthcare providers in supporting male victims/survivors of sexual violence, including survivor-centred approaches to care, and any barriers in the provision of this care. Overall, despite few healthcare providers having provided services to male victims/ survivors, the majority of healthcare providers interviewed had knowledge of the characteristics of a survivorcentred approach to healthcare and were able to articulate how they would put this into practice. Further, their descriptions of how to implement such an approach were largely in line with the guidance provided in the GBV Treatment Protocol for Healthcare Providers in Afghanistan despite only a small proportion of healthcare providers having been trained in the use of the Protocol and the Protocol being largely framed around the needs of women and girls. Despite healthcare providers’ overall knowledge of survivor-centred care, there is significant dissonance between their descriptions of the care they would provide to a male victim/survivor, and the treatment that male victims/survivors expect to receive. This could be due to victims/ survivors being unaware of more recent advancements in health sector responses to GBV more generally. However, it may also be due to persisting gaps in healthcare providers’ attitudes, knowledge and practices with regards to male victims/survivors of sexual violence.
One of the most important healthcare needs of male victims/survivors of sexual violence is to be treated with no judgement, blame or stigma. Victims/survivors also strongly emphasised the importance of confidentiality and the need to trust that a healthcare provider would not disclose their case to family or community members and, importantly, judicial actors, without their consent. Healthcare providers also emphasized the importance of these principles of care; however, it is unclear the extent to which they are implemented in practice. The research findings suggest that some healthcare providers may reproduce blame or stigma when male victims/survivors of sexual violence engage in sex work or if they identify as having diverse SOGIESC. Further, the research points towards a possible gap in healthcare providers’ recognition of male victims/survivors with diverse SOGIESC as a vulnerable group in need of services, or as legitimate victims/survivors of sexual violence. This lack of recognition may be due to assumptions that male victims/ survivors with diverse SOGIESC who access health facilities for sexual violence have in fact consented to sexual acts and, thus, that these cases should be classed as sodomy, which is illegal under the Afghan Penal Code. It is unclear from the research what kinds of legal provisions healthcare providers are required to abide by with regards to male victims/survivors of sexual violence, including respect for confidentiality and rights to instigate the criminal justice process or not. Although the GBV Treatment Protocol articulates legal provisions for female survivors under the EVAW Law, the Protocol does not articulate the rights of male victims/survivors of sexual violence.
Another important gap in healthcare providers’ knowledge, practices and capacities is related to the age of victims/survivors. Healthcare providers did articulate barriers that boy victims/survivors of violence particular faced in accessing healthcare services, including lack of knowledge of how to access a facility. However, healthcare providers appeared to lack awareness of the different needs of adults and children, and understanding of how the evolving capacities of the child should be integrated into healthcare response. This may be due to the majority of healthcare providers interviewed never having provided services to male victims/survivors of sexual violence, whether boys or adults. However, lack of understanding of or capacity to implement an approach that recognises the evolving capacities of the child was also found among healthcare providers who reported having provided services to girl victims/survivors of sexual violence, suggesting that there is a broader gap in this area.
The research has identified a number of other gaps in the provision of healthcare services to male victims/ survivors of sexual violence. Healthcare providers emphasized the unavailability of psychosocial services for victims/survivors of violence, and the lack of capacity of psychosocial counsellors to deliver services specifically to male victims/survivors of sexual violence.
REFERENCES
Afghanistan Analysts Network, Widespread Violence yet Perpetrators go Unpunished: A New UN report on Violence Against Afghan Women, 29 May 2018 (updated 9 March 2020), http://bit.ly/3cmN7LO.
Afghanistan Independent Human Rights Commission, National Inquiry Report on Factors and Causes of Rape and Honor Killing in Afghanistan, August 2015, https://bit.ly/3eyjcmg.
Afghanistan Independent Human Rights Commission, Causes and Consequences of Bacha Bazi in Afghanistan (National Inquiry Report), August 2014, https://bit.ly/3lhJieL.
Afghanistan Independent Human Rights Commission, Summary of the Report on Violence Against Women. The Causes, Context, and Situation of Violence Against Women in Afghanistan, March 2018, www.refworld.org/docid/5ab132774.html.
Afghanistan Independent Human Rights Commission, Monitoring and Investigation of Alleged Child Sexual Harassment in Schools and Workplaces in Logar Province, January – February 2020, www. aihrc.org.af/home/research_report/8801.
Afghanistan Public Policy Research Organization, New Penal Code and EVAW Law: To Incorporate or Not to Incorporate? July 2018, https://bit.ly/38y3fci.
All Survivors Project, The Health of Male and LGBT Survivors of Conflict-Related Sexual Violence, 2020. https://bit.ly/30DKYWw.
Anbrasi Edward et al., ‘Toward Universal coverage in Afghanistan: A multi-stakeholder assessment of capacity investments in the community health worker system’, Social Science & Medicine, 145: 173-183, 2015, http://bit.ly/3qKQS2C.
Anne Gatuguta et al., ‘Should community health workers offer support healthcare services to survivors of sexual violence? A systematic review’, BMC International Health and Human Rights, 17: 28, 2017, http://bit.ly/3qFdnWH.
ARC International, International Bar Association’s Human Rights Institute, and International Lesbian, Gay, Bisexual, Trans and Intersex Association, Sexual Orientation, Gender Identity and Expression, and Sex Characteristics at the Universal Periodic Review, November 2016, https://bit.ly/3ez2Z07.
Central Statistics Organization (CSO), Ministry of Public Health (MoPH) and ICF International, Afghanistan Demographic and Health Survey 2015, January 2017, https://bit.ly/2OooHJC.
Dominique Day & Abdul Rasheed, Assessing the Readiness and Capacity of Health Facilities and Health Care Providers to Strengthen Health Response to Gender-Based Violence in 14 Provinces of Afghanistan, 2018.
Gender-based Violence Information Management System Steering Committee, Interagency Gender-Based Violence Case Management Guidelines. Providing Care and Case Management Services to Gender-Based Violence Survivors in Humanitarian Settings, First Edition, 2017, http://bit.ly/2Nd6lLh.
Islamic Republic of Afghanistan Ministry of Justice, Justice Sector Support Program Translation of the Final Version of the Penal Code, September 2017.
Islamic Republic of Afghanistan Ministry of Justice, Law on Protection of Child Rights, March 2019, https://uni.cf/3evdPUX.
Islamic Republic of Afghanistan Ministry of Public Health, GenderBased Violence-Psychosocial Counseling Training Packages. Module 1: Understanding Gender-Based Violence, undated, , https://bit.ly/3vk3Rf1.
Islamic Republic of Afghanistan Ministry of Public Health, A Basic Package of Health Services for Afghanistan, 2009.
Islamic Republic of Afghanistan Ministry of Public Health, World Health Organization and United Nations Entity for Gender Equality and the Empowerment of Women (UN Women), Gender-Based Violence Treatment Protocol for Healthcare Providers in Afghanistan, 2014, http://bit.ly/3lau9fa.
Julienne Corboz & Zulaikha Rafiq, Localisation for GBV prevention and response in Afghanistan: A policy study in support of CARE’s Voices and Partnerships against Violence (Safe from the Start) Project, CARE UK, 2019.
Medica Afghanistan/medica mondiale, GBV and Trauma-Sensitive Healthcare in Afghanistan: A Baseline Study, September 2016, https://bit.ly/30C8WBt.
Médecin Sans Frontières, Between Rhetoric and Reality: The Ongoing Struggle to Access Healthcare in Afghanistan, February 2014, http://bit.ly/38ygTvH.
MOSAIC (MENA Organisation for Services, Advocacy, Integration and Capacity Building), Male Survivors of Sexual Assault: A Manual on Evaluation and Management for General Practitioners, undated, https://bit.ly/3lbtJ8l.
Naz Foundation International, Rapid Assessment of Male Vulnerabilities to HIV and Sexual Exploitation in Afghanistan. Final Report, 30 March 2009, https://bit.ly/3bHyu6u.
Said Ahmad Maisam Najafizada, Ivy Lynn Bourgeault & Ronald Labonté, ‘A gender analysis of a national community health workers program: A case study of Afghanistan’, Global Public Health, 14(1), 2019.
Sarah Chynoweth et al., ‘A social ecological approach to understanding service utilization barriers among male survivors of sexual violence in three refugee settings: a qualitative exploratory study’, Conflict and Health, 14: 43, 2020, http://bit.ly/3vk52uX.
Save the Children, Knowledge, Attitudes and Practices on Violence and Harmful Practices Against Children in Afghanistan: A Baseline Study, August 2017, https://bit.ly/2PMI8fx.
Save the Children and Federal Republic of Germany Foreign Office, Learning Without Fear: A Violence-Free School Project Manual, 2011.
Terre des Hommes, An Assessment of Juvenile Justice in Afghanistan, January 2010, https://bit.ly/2Oo6pIs.
United Nations International Children’s Emergency Fund (UNICEF), Children and Women in Afghanistan: A Situation Analysis, November 2014, http://uni.cf/30zsvKK.
United Nations Office on Drugs and Crime, Afghanistan: Implementing Alternatives to Imprisonment, in line with International Standards and National Legislation. Assessment Report, May 2008, https://bit.ly/2ONUjZf.
United Nations Population Fund, Knowledge, Attitudes and Practices Survey on Gender-Based Violence in Five Provinces in Afghanistan, 2016.
United Nations Security Council Report of the Secretary-General, Conflict-Related Sexual Violence, S/2015/203, 23 March 2015.
United Nations Security Council Report of the Secretary General. Children and Armed Conflict in Afghanistan, S/2019/727, 10 September 2019.
Vu et al., Integrated Behavioral and Biological Surveillance in Afghanistan: Findings of 2012 IBBS Survey and Comparison to 2009 IBBS Survey (unpublished), 2013, cited in Andrea Wirtz et al., ‘Uncovering the epidemic of HIV among men who have sex with men in Central Asia’, Drug and Alcohol Dependence, 132 Suppl 1: S17-24, 2013, https://bit.ly/30BYzgT.
Women’s Refugee Commission, “It’s Happening to Our Men as Well”: Sexual Violence Against Rohingya Men and Boys, November 2018, http://bit.ly/3qIFxAf.
Women’s Refugee Commission, “More Than One Million Pains”: Sexual Violence Against Men and Boys on the Central Mediterranean Route to Italy, March 2019, http://bit.ly/30BYHwT.
World Health Organization, Responding to Children and Adolescents who have been Sexually Abused: WHO Clinical Guidelines, 2017, http://bit.ly/3coiXYy.
World Health Organization and Youth Health and Development Organization, Assessment on the capacity of health facilities and health care providers to respond to gender-based violence in Afghanistan. Baseline Assessment, 2015.
ANNEX A: METHODOLOGY
Objectives
The objectives of the research were to:
- Understand the healthcare experiences and needs of male victims/survivors of sexual violence and the barriers to their access to quality healthcare services.
- Understand the practices of healthcare providers in relation to supporting male victims/survivors of sexual violence and the barriers they face in providing quality healthcare services to them.
- Understand what a survivor-centred approach to healthcare provision means, and how it is applied in Afghanistan, with regards to male victims/survivors.
- Develop a set of recommendations for enhanced survivor-centred healthcare services for male victims/ survivors of sexual violence that will be used to develop a tool for the health sector.
The third objective, related to survivor-centred healthcare, was nested within the research as part of a wider ASP research project implemented in four countries. The data specifically collected to address this objective will be reported as part of the wider multi-country study, and are included in this report insofar as they address the first, second and fourth objectives.
Research Approach
The overall research approach was qualitative in order to understand the perceptions and lived experiences of male victims/survivors of sexual violence as they navigate the barriers and enablers of access to quality healthcare services in Afghanistan, and of the healthcare providers who provide these services.
The main qualitative methods employed in the research were based on a storytelling approach in which a vignette/story of a male victim/survivor of sexual violence was used to prompt storytelling and discussion whereby different types of participants were asked to discuss the story through the eyes of the victim/ survivor. The use of a vignette approach served a number of purposes.
- Using this kind of methodology can give victims/survivors more control over whether and how they wish to share information about their own experiences. This can often lead to victims/survivors feeling more open to tell their own stories but through their own choice rather than a forced interview guideline. Although victims/survivors were asked to imagine a particular scenario and provide their perspective on that scenario, they were free to speak about their own stories if they wished to. If they didn’t choose to speak about their own experiences, this was on their terms and not because they felt compelled to because of how the interview was structured.
- Asking various actors to imagine a scenario from the perspective of a victim/survivor provides an opportunity to encourage a survivor-centred perspective by asking participants to imagine a scenario and series of events through the eyes of a victim/survivor.
- It was recognised during the inception period that many victims/survivors may not have accessed healthcare services for sexual violence they had experienced. Likewise, it was recognised that many healthcare providers will not have provided support to male victims/survivors of sexual violence. Consequently, asking direct questions about experience may have yielded limited results. In the absence of having accessed or delivered healthcare services, the use of a hypothetical scenario provided a foundation to start a discussion about the needs of male victims/survivors of sexual violence and how these should be met.
Methods
Desk Review
A desk review was conducted, including literature on sexual violence against men and boys and health sector response, with a focus on evidence from Afghanistan. The desk review formed the basis for the design of the research approach, including identifying key gaps in evidence.
Stakeholder Mapping
A stakeholder mapping was conducted to identify existing systems of healthcare response that include coverage of male victim/survivors in Afghanistan, predominantly through a desk review of online documents. A selection of stakeholders was then invited to participate in key informant interviews (KIIs).
Key Informant Interviews with Stakeholders
KIIs sought to understand the key organisations and actors working to provide healthcare services to male victims/survivors of sexual violence, including in the sampled provinces. They also sought to understand how organisations’ care models and pathways, and operational strategies, address the needs of victims/survivors of sexual violence, including female and male, and the institutional, systemic and contextual barriers and enablers to providing health services to male victims/survivors of sexual violence in particular.
In-Depth Qualitative Interviews
The fourth method comprised in-depth interviews (IDIs) with (1) male victims/survivors of sexual violence, (2) healthcare providers working in different types of healthcare settings and (3) community health workers (CHWs). The second and third categories have been established to account for the fact that healthcare services for victims/survivors in Afghanistan are broadly separated into static services and outreach services. However, it is recognised that CHWs provide very limited services and are more likely to refer victims/survivors to healthcare facilities than provide treatment or psychosocial support themselves.
Three different qualitative tools were developed for each type of participant, and all three were harmonised to draw from the same approach. All three tools were divided into three components:
- A vignette to explore the barriers that male victims/survivors of sexual violence face in accessing healthcare.
- A continuation of the vignette to facilitate a walk through a healthcare pathway to explore what occurs when a male victim/survivor accesses services at a healthcare facility or through a community health worker.
- A series of questions about what is needed to improve healthcare services for male victims/survivors.
These three components are described more fully below, with the tools included in Annex B.
In the first component of the qualitative tools, the interviewer reads out a hypothetical scenario that involves sexual violence perpetrated against a male victim/survivor who does not access health services (see Box 10). The vignette is accompanied by a series of questions or probes about the hypothetical scenario, why the victim/survivor does not want to access health services and the barriers that he might face in doing so. The questions and probes for this component of the tool are the same for all three types of participants, allowing an analysis of how different actors perceive the context of violence and the barriers for male victims/survivors.
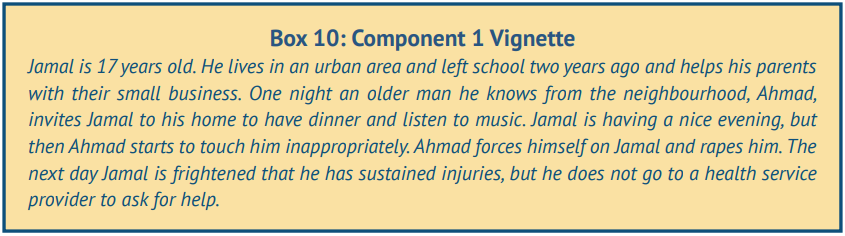
In the second component of the qualitative tools, the interviewer continues the hypothetical scenario, in which the victim/survivor decides to access health services (e.g. a health facility) or support (e.g. through a community health worker). The interviewer guides participants through what the victim/survivor would experience at different stages of the care or support pathway through a series of probes designed to elicit participants’ perspectives through the eyes of the victim/survivor.[47] The context and probes differ according to the participant.
- Victims/survivors are asked to describe a hypothetical scenario in which the male victim/survivor (Jamal) accesses a health facility. Probes are related to reflections on the different types of staff or actors the victim/survivor comes into contact with at different points of the care pathway, and whether the victim/survivor feels supported, respected and in control of health decision making.
- Healthcare providers are asked to describe a hypothetical scenario in which the male victim/survivor (Jamal) accesses their health facility, and are asked to describe what the care pathway would be. Probes are related to reflections on which staff members would interact with the victim/survivor at different points in the care pathway, how they treat the victim/survivor, and existing procedures and protocols for handling cases of sexual violence, including sexual violence against men and boys.
- Community health workers are asked to describe a hypothetical scenario in which the male victim/ survivor (Jamal) seeks support from a community health worker, with probes related to how the health worker would support the victim/survivor and how equipped they would feel to do so.
In the third component of the qualitative tools, participants are asked questions about their own experiences accessing healthcare services (victims/survivors) or delivering healthcare services (healthcare providers and community health workers). This component of the tool also explores victim/survivor needs in relation to accessing services and healthcare provider needs and capacities to deliver high quality health services that are responsive to the lived experiences of male victims/survivors.
Piloting of Tools
The three qualitative tools with victims/survivors, healthcare providers and CHWs were piloted prior to fielding the data collection. Each tool was piloted twice (a total of six pilot interviews), with a spread of interviews piloted in each province and healthcare provider and CHW tools piloted with both women and men. The tools were piloted in Dari in Balkh, Pashto in Kandahar and both Dari and Pashto in Kabul depending on the first language of the respondent.
During the pilot with male victims/survivors, after completing the interviews the research assistants consulted participants on the content of the tool and appropriateness of the story narrative and questions to ensure that the tool was respectful and accurately represented the experiences and needs of male victims/survivors.
Some minor modifications were made to the tools as a result of the pilot, including the simplification of language for some questions where participants struggled with comprehension. The tools were also shortened due to some duplication in questions and the finding that the interviews were too long, leading to concerns about interview fatigue.
Due to the main questions in the tools being retained with little change in the meaning, the pilot interviews were included in the sample of interviews analysed.
Sampling
The research was implemented in three provinces, Kabul, Balkh and Kandahar. These provinces were selected in order to capture data from three geographical regions of the country (central, northern and southern) and also due to YHDO’s presence in these regions.
Table 2 contains a summary of the research sample for qualitative interviews with stakeholders, victims/ survivors, healthcare providers and CHWs (including pilot interviews). A total of 107 interviews were conducted, including 97 in-depth interviews and 10 key informant interviews. The sampling approach for each type of participant is described further below.
Table 2: Qualitative Sample
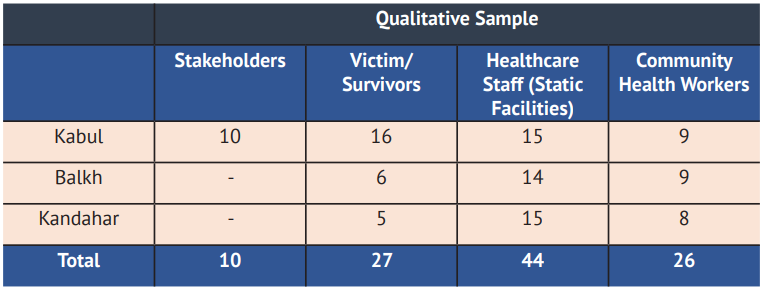
Stakeholders
The research team had originally planned to conduct 20 KIIs with stakeholders, including government stakeholders, national and international NGOs, UN agencies, and stakeholders specifically linked to relevant clusters or networks, including the GBV sub-cluster and the CPAN. Due to challenges arranging interviews (see section on challenges and limitations), 10 KIIs were completed with stakeholders from the following organisations.
- The Gender Directorate of the MoPH
- The Afghanistan Independent Human Rights Commission (AIHRC)
- Three UN agencies – UNAMA, UNFPA and WHO
- Three national NGOs, including Bu Ali Rehabilitation & Aid Network (BARAN), Medica Afghanistan and Sanayee Development Organization (SDO)
- International Medical Corps (IMC)
- The North Atlantic Treaty Organization (NATO)
Victims/survivors
A total of 27 male victims/survivors of sexual violence were sampled: 16 in Kabul, six in Balkh and five in Kandahar. Due to ethical reasons, only victims/survivors aged 18 years or above were sampled. The mean age of victims/survivors sampled was 25, with an age range of 18 to 40 years. Due to the focus of the research on access to healthcare services, victims/survivors were not asked directly about their experiences of sexual violence in the past; however, four victims/survivors did explicitly refer to being raped as children. Consequently, although the research sampled adults, the research team was able to conduct some retrospective analysis of the experiences of boys. Victims/survivors were not asked to self-identify their SOGIESC as the research team did not want to risk participants feeling stigmatised. Hence, it is unknown the extent to which the victims/survivors sampled have diverse SOGIESC given that only two victims/survivors, unprompted, openly identified as gay. However, six other victims/survivors referred to men and boys who were gay or transgender, or who had ‘female specifications’, being particularly vulnerable to sexual violence, and described the barriers that victims/survivors with diverse SOGIESC would face accessing healthcare services. Consequently, the research team was able to extract some data on the experiences of victims/survivors with diverse SOGIESC.
YHDO contacted victims/survivors from their list of beneficiaries who have accessed their services at the provincial level, and who have developed a relationship with the organisation, either as staff members, advocates, peer mentors or in other support roles. Only victims/survivors known by YHDO to not currently be in a situation of harm or sexual exploitation were invited to participate in the research. Due to the data collection approach with victims/survivors (see the section on remote data collection further below), male victims/survivors were all sampled in the provincial centres and those living in non-central districts and rural areas were not sampled.
While the research team acknowledges that the sampling approach outlined above may have introduced some bias, there were a number of reasons for sampling victims/survivors with an established relationship with YHDO. It was reasoned that they were less likely to be at risk of reliving trauma or under current sexual exploitation given they had adopted support roles within YHDO. Further, given they have established a trusting relationship with YHDO, it was reasoned that it was more likely they would feel they could openly share their perceptions with trusted YHDO interviewers. The larger sample of victims/survivors in Kabul than in Balkh and Kandahar was due to a larger number of victims/survivors in Kabul fulfilling the criteria for inclusion in the research.
Healthcare Providers in Static Facilities
In order to capture different types of healthcare facilities in both urban and rural areas, the research aimed to sample seven static healthcare facilities per province, including: provincial or regional hospitals, FPCs located in provincial or regional hospitals, private hospitals, district hospitals, CHCs, BHCs and HSCs. Provincial and regional hospitals, including FPCs, and private hospitals, were sampled in provincial centres. The research team drew a random sample of four districts, covering both urban and rural districts, from which to sample district hospitals, CHCs, BHCs and HSCs.
The research team aimed to sample three types of healthcare providers per facility in provincial/regional and district hospitals and in private health facilities, including a:
- Healthcare Worker: A healthcare provider in a medical support role who may be the first focal point for victims/survivors (e.g., nurse, midwife, male health educator)
- Medical Practitioner: A healthcare provider in a more specialised medical role (e.g., medical doctor, surgeon, emergency physician, paediatric doctor)
- Mental Health and Psychosocial Support Staff: A healthcare provider providing counselling or psychosocial support.
The research team aimed to sample two healthcare providers per FPC, including a medical doctor and psychosocial counsel[48] , and one healthcare provider per CHC, BHC and HSC given that these are smaller health facilities with fewer staff. In these smaller health facilities, the aim was to distribute the sample across different types of healthcare providers, including healthcare workers, medical practitioners and mental health specialists, with the addition of clinic managers, keeping in mind that these health facilities (particularly BHCs and HSCs) are likely to be staffed mainly by clinic managers, nurses and midwives. The research aimed to sample a balance of male and female healthcare providers across the different types of healthcare facilities. It should be noted that although healthcare providers in FPCs have the specific role of providing services to GBV victims/survivors, the healthcare providers sampled across the other types of health facilities serve the general population, who may or may not include GBV victims/survivors. Hence, the research team was not able to sample healthcare providers in specialised GBV roles given that these roles don’t exist in the BPHS and EPHS system outside of FPCs.
Interviewers received a list of healthcare facilities and healthcare providers from the MoPH, drew a sample based on the parameters outlined above and contacted healthcare providers to invite them to participate in interviews. The target sample of 14 healthcare providers per province was met, with a total of 44 interviews conducted. Although the research team had initially planned to balance the gender of healthcare providers, female healthcare providers were more difficult to sample in some facilities given that staff were predominantly men. Further, there were more refusals from female healthcare providers than for male providers. Consequently, the sample of male healthcare providers is greater (n=28) than female healthcare providers (n=16). Given that male victims/survivors of sexual violence are more likely to have received services from male healthcare providers than female providers, the larger sample size of male healthcare providers was not considered a limitation in the research.
The number of healthcare providers sampled per type of health facility varied from the target (see Table 3). Notably, HSCs were not sampled, healthcare providers from FPCs were only sampled in Kandahar, and some types of healthcare facilities were either under- or over-sampled. There were also some gaps in the types of healthcare providers sampled, including few mental health specialists (see Table 4). Further details on reasons for these gaps are noted in the section below on challenges and limitations.
Table 3: Number of Healthcare Providers Sampled Per Health Facility, Per Province
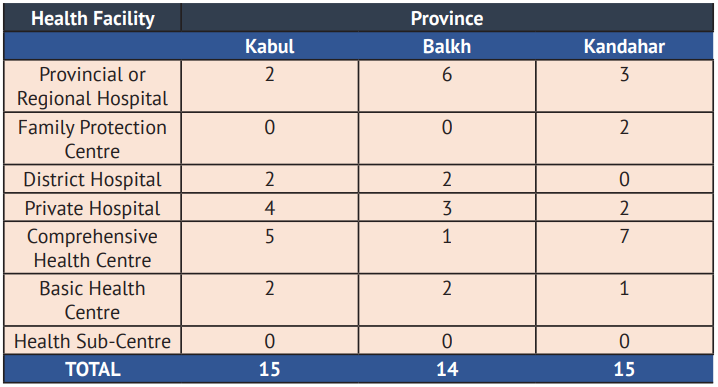
Table 4: Type of Healthcare Providers Sampled Per Province
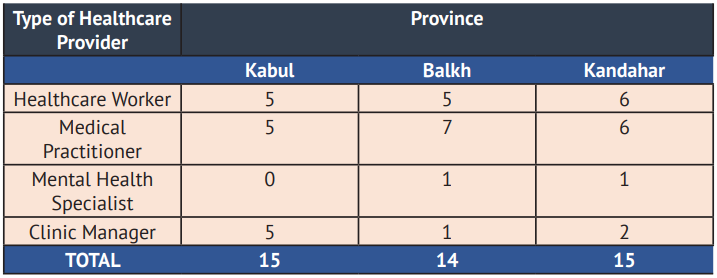
Community Health Workers
The original target sample for CHWs was one male and one female CHW per district, with two randomly selected districts sampled per province (one urban or semi-urban district and one rural district), with a total of 12 CHW interviews (four per province). In addition, the original research proposal had planned to incorporate 12 interviews with mobile outreach workers who provide mobile health services to more remote communities where there is a lack of static facilities. After internal discussions between ASP and YHDO, it was decided to drop the mobile outreach worker interviews and instead sample additional CHWs due to concerns that mobile outreach workers would not have sufficient information about the healthcare needs of male victims/survivors, or providing services to them.
The research team obtained CHW contact details from the MoPH and drew a random sample of CHWs from selected districts and invited them to participate in an interview. As outlined above for healthcare providers, the research team had challenges recruiting female CHWs including more refusals. Much like for healthcare providers, this was not considered to be a major limitation given that male CHWs are more likely than female CHWs to be a focal point for seeking referrals to access healthcare facilities. A total of 26 interviews were conducted with CHWs, including eight female and 18 male CHWs.
Remote Data Collection
At the start of the inception period for the research, the COVID-19 pandemic had begun to spread leading to risk mitigation procedures being implemented at the global level, including in Afghanistan. These included lockdowns and social distancing to minimise transmission of the virus. As a result, it was decided that all data collection for the research would be done remotely via telephone interviews in order to protect both the participants and researchers.
A remote data collection approach was employed for interviews with healthcare providers and CHWs. However, the research team had concerns about how to ensure the confidentiality and privacy of victims/survivors if conducting telephone interviews in which interviewers would not be physically present to ensure a private space could be found and negotiated throughout the interview. Of particular concern was the possibility that victims/survivors might disclose experiences of violence while family members or others (including perpetrators) were present or could overhear the interview, putting victims/survivors at risk of further violence.
In order to mitigate risk to victims/survivors, a hybrid approach was employed. Victims/survivors were invited to access a YHDO office in Kabul, Mazar-e Sharif (Balkh province) or Kandahar City where they were provided with a private space with the necessary telephone or internet technology to participate in an interview facilitated remotely. Precautions were made to ensure a safe environment for victims/survivors (see further detail in the section on ethical approach).
Data Processing and Analysis
Qualitative interviews were transcribed and translated from Dari and Pashto to English. All transcripts were coded using the application Dedoose and analysed thematically. This was done according to an inductive thematic coding approach, which uses free or open coding to produce theories about a phenomenon from the ground up. In contrast, deductive coding uses theory as a starting point and develops a set of established codes from which to work. The latter approach is usually used when conducting evaluations with a determined set of evaluation questions, or when conducting research on a topic that much is known about and the research has a specific set of questions and targeted areas of knowledge. Given that there has been very little documented on male victim/survivors’ access to healthcare services in Afghanistan and the barriers they face, an inductive coding approach was more appropriate to ensure that unexpected phenomena were captured.
Ethical Approach
The research was conducted in line with an ethical, safe and survivor-centred approach. Ethical approval was obtained from the Institutional Review Board of the MoPH in Afghanistan according to the protocols outlined below.
No male victims/survivors under the age of 18 were sampled for the research. This was primarily due to the additional risks of interviewing children. It was reasoned that boy victims/survivors may be more at risk of currently being in a situation of sexual exploitation or abuse, such as bacha bazi. Further, obtaining consent from parents or caregivers of children may have placed victims/survivors at risk of further harm, particularly in cases where parents are unaware of the sexual violence children have experienced.
All participants were required to provide informed consent before participating in interviews. Given that the data collection was done remotely, written consent could not be obtained and, instead, interviewers followed consent procedures on the telephone call before starting interviews. Interviewers read out the consent plain language statement (see the content of these statements before the interview tools in Annex A) and obtained verbal consent from participants, both to participate in the interview and have the interview audio recorded. In case where participants consented to participate in the interview but not have the interview audio recorded, interviewers took detailed notes of the content of the interview.
It is important when conducting interviews with victims/survivors of violence that this is done in privacy. As outlined previously, this was ensured by implementing a hybrid approach whereby victims/survivors accessed YHDO offices and were provided with a safe and private room in which to participate in a telephone interview. The research team developed a safety and COVID-19 risk mitigation strategy involving the following procedures:
- Victims/survivors were supported to access and leave YHDO offices through safe transport.
- All staff at YHDO offices wore masks, used hand sanitiser and maintained social distancing when greeting victims/survivors and showing them to interview rooms.
- Victims/survivors were also provided masks and hand sanitiser and briefed on YHDO office COVID-19 risk mitigating procedures.
- Interview rooms and equipment (phones, computers, headphones) were disinfected after each victim/ survivor interview.
Confidentiality for participants was ensured by de-identifying transcripts and removing names, names of healthcare facilities or organisations and district names from the report generated from the study. For those interviews that were audio recorded, interview files were downloaded onto a computer and stored in a password protected folder. Once interviews had been downloaded, audio files were deleted from the phone or digital recording device. After transcription and translation of interviews, and monitoring and quality checks conducted by YHDO, audio files were deleted.
It is possible that male victims/survivors will relive trauma when discussing the topic of violence or if they disclose their experiences of violence to interviewers. In order to mitigate this risk, before starting interviews the research team briefed victims/survivors about the availability of YHDO counselling if they felt upset or distressed as a result of their participation in the interview. Interviewers reminded victims/survivors of the availability of these services if they showed signs of distress during the interview.
The research team participated in ethics and safety training, including on ensuring privacy and confidentiality, obtaining informed consent without coercion, respecting the withdrawal of consent at any time, ensuring respect for victims/survivors at all times, recognising signs of distress and handling disclosures of violence.
Challenges and Limitations
The research team faced a number of challenges implementing the research, leading to some limitations, as outlined below.
A key challenge was accessing participants. Some stakeholders were difficult to reach and did not return emails and follow up emails inviting them to participate in stakeholder KIIs. One stakeholder responded to emails but appeared to be concerned about the topic and how the information would be used and wanted some control over how the data would be reported.
The research team also faced significant challenges sampling healthcare providers. The MoPH did not provide contact details for healthcare providers in HSCs and so the research team had to increase the number of interviews in other types of facilities. For other types of healthcare facilities, many of the phone numbers provided by the MoPH did not work, or interviewers repeatedly found phones to be switched off. Some healthcare providers refused to participate as they were too busy and were discouraged when interviewers told them about the estimated length of the interview (one hour). Healthcare providers from some facilities also refused to cooperate with the research team despite the necessary approvals being obtained from the MoPH. Due to time constraints and the need to fulfill fieldwork deadlines, the research team adjusted the sample by increasing interviews in facilities where providers were more responsive to participation in the research. In some cases, this also meant adjusting the district sampled.
The research aimed to sample FPC healthcare providers given that FPCs are central facilities for the delivery of services to victims/survivors of violence (albeit generally women and girls). FPCs were only sampled in one province due to some confusion among interviewers in Kabul and Balkh about what constitutes an FPC. However, this gap has been partially filled by the inclusion of a stakeholder interview with a representative of an NGO implementing FPC services.
Interviewers faced a number of challenges using a remote, telephone-based data collection approach with healthcare providers and CHWs. Participants’ poor telephone connections and batteries running out led to disruptions in interviews. In some cases, interviewers were unable to recontact participants and continue interviews, and had to sample new participants.
Only one CHW reported having provided support to male victims/survivors. Although the CHW data was useful insofar as CHWs are widely recognised as a possible entry point to male victim/survivors’ access to healthcare facilities through referrals, CHWs had little awareness or knowledge about male victims/survivors of sexual violence or their needs. Conversely, although a choice was made to drop mobile outreach workers from the sample, when analysing the data it became apparent that mobile outreach workers may be a key entry point for victims/survivors to access referrals to healthcare facilities, and one that is being used. The gap in perspectives of mobile healthcare providers is thus a limitation in the research.
Only seven male victims/survivors (one quarter of those interviewed) reported having accessed non-YHDO healthcare facilities for sexual violence they had experienced in the past. Further, only nine healthcare providers (one fifth of those interviewed) reported having provided services to male victims/survivors of sexual violence. This challenge was expected and difficult to avoid given the substantial barriers male victims/ survivors face accessing healthcare services, and was one of the reasons for using a hypothetical vignette approach in the interview tools. Consequently, much of the data is based on perceptions or, in the case of victims/survivors, what they have heard from other victims/survivors, rather than direct personal experience.
Given that all victims/survivors interviewed were adults, there is an important gap in the research on the experiences of boys. The research team was able to analyse some data retrospectively where male victims/ survivors disclosed that they had experienced sexual violence at a young age. Further, of the nine cases in which healthcare providers reported that they had provided services to male victims/survivors in the past, five referred to providing services to boys, also allowing additional learning about healthcare response to boy victims/survivors of sexual violence. However, the lack of direct data collected on child and adolescent boy experiences of accessing healthcare services is a gap that is important to address in future research.
ANNEX B: QUALITATIVE TOOLS
Key Informant Interviews with Stakeholders
Hello. My name is __________ and I am working with the All Survivors Project (ASP) and Youth Health and Development Organization (YHDO). We are conducting interviews with key stakeholders in the health, protection and GBV response sectors. Women, men, girls and boys can experience gender-based violence in Afghanistan, with women and girls particularly at risk. We recognise the continuing need to address the needs of female survivors of GBV, and would like to understand how the current services available for female survivors can grow, be improved and also address the needs of male survivors of sexual violence.
- In Afghanistan, what key policies, legislation, or law(s) exist to address sexual violence against men and boys?
- Currently, what is the key role of the health sector in Afghanistan in responding to sexual violence against men and boys? (Prompt for healthcare facilities – What packages of care are available for survivors in this health facility?)
- What other sectors are working to address sexual violence against men and boys?
- What barriers does the health sector face in providing services to male survivors of sexual violence? What is the health sector doing to respond to these challenges?
- What kinds of resources, protocols, trainings or manuals are currently available to support health staff to provide better treatment and health care to male survivors of sexual violence? How effective are these resources/protocols in addressing the needs of these survivors?
- Is there demand in the health sector to build and improve resources, protocols, manuals and services to address the needs of male survivors of sexual violence?
- Are there any mechanisms in place in your work setting to ensure that male survivors of sexual violence have access to quality health care? (Prompt: this could be operating procedures, policies, etc)
- What kinds of challenges have you faced in implementing these mechanisms? (Probe on different types of barriers – human resources and staff turnover, material resources, lack of equipment, knowledge/ capacity, etc)
- Have you heard of the term “survivor-centred approach” to healthcare service provision before? (If yes, what does this mean to you? If no, what do you think it might mean?)
- What makes services survivor/centred? How can healthcare providers be survivor-centred in their service design and provision?
- For healthcare staff to be survivor-centred, what kinds of skills do they need? What kinds of attitudes do they need?
- How does survivor-centred healthcare response for female survivors differ from survivor-centred response for male survivors?
- Do you know of any other organisations working on responding to sexual violence against men and boys who we should speak with?
Key Informant Interviews with Male Survivors of Sexual Violence
Consent Form for Survivors of Sexual Violence
Hello. My name is __________ and I am working with the All Survivors Project (ASP) and Youth Health and Development Organization (YHDO). We are conducting interviews to collect information on the experiences and perspectives of male survivors of sexual violence. We are interested in understanding your experiences attempting to access healthcare services for violence that you have experienced, the barriers that you have faced trying to access these services and how healthcare practitioners can better address your needs. If you have never accessed health services for violence, we would still like to hear your thoughts about the barriers that survivors face and how healthcare providers can provide support.
The findings from this interview will be used to understand the readiness and requirements of the health sector to strengthen healthcare response to sexual violence against men and boys. There are no direct benefits to you by participating in this interview, although your help in responding to these questions will be used to help healthcare providers deliver better services to male survivors of violence. Even if you have not accessed healthcare services for violence you have experienced, your perspective is still very important as we need to better understand the barriers that male survivors face in accessing services.
Due to the sensitivity of the topic, you might experience discomfort during the interview. Sometimes when survivors of violence speak about violence, they can relive some of the trauma they felt. If you feel uncomfortable or upset at any time, you can pause or stop the interview. If you feel that you need to speak with a counselor, please let me know as there is a counselor who I can arrange to call you on the phone and provide free and confidential counseling. We will also provide you with a list of medical or counseling services that you can access if you wish.
You can decide to skip any questions that you do not want to answer, and you are free to withdraw your participation at any time, without giving a reason. If you do refuse to answer a question or if you decide to withdraw your participation in the interview, nobody will be upset with you and this will in no way affect your ability to access help from a counselor or from other medical or counseling service providers. Your answers will be confidential. I would like to audio record the interview so that I can capture our discussion correctly. After I have transcribed the interview, we will delete the audio recording. If you would prefer that I did not audio record the interview, then I can take notes of our discussion.
Your name will not be included in the transcripts or any reports that we write about this study. We will analyse the data from this interview alongside the interviews of other survivors of violence. The only people who will have access to the anonymized interview transcript or notes are the people who are working on this study. Nobody else will know what we have spoken about.
If you would like more information about this study, or if you would like to complain about this interview or any part of the research, you can contact Dr Rasheed the director of YHDO on (Tel: ———-). If after our interview you feel upset or start to relive any trauma from or stress linked to violence you have experienced, you can also contact Dr Rasheed so that YHDO can arrange for a counselor to call you.
The interview will take approximately 1.5 hours. If you have any questions, you can ask now, or at any point during our discussion or at the end of the interview. Do you have any questions about the study?
Do you consent to participate? Do you consent to have the interview audio recorded? Do you consent for us to use quotes from this interview in our report (these quotes will be anonymous and we will not use your name)?
(Guidance – if the person does not consent to participate then politely thank them for their time and end the consent process. Also ask them if they would like to access any services for survivors in their area and provide these details accordingly. If the person consents to participate and have their interview recorded, proceed by beginning the audio recording and the interview. If the person consents to participate in the interview but does not want the interview audio recorded, then take notes of the discussion. Before starting the interview, emphasize the importance of the interview taking place in a private setting as outlined below. When being contacted with an invitation to participate in the interview, the survivor will already have been briefed on the need to conduct the interview at a time when there is privacy, but it important to ensure that this is being upheld prior to starting the interview).
Because of the sensitivity of the topic, it is important that we have privacy when we speak and that nobody else is present during our interview. This is to make sure that your privacy is respected and so that we can ensure that you are safe from harm. If anybody interrupts the interview or if there is a situation where somebody else is present during the interview, then I would like you to let me know so we can stop or pause the interview. If it is difficult to find a private location, we can arrange another time for me to call you.
Interview Guidelines for Survivors of Violence
- Province: __________________________________________________________
- District: __________________________________________________________
- Age of participant: __________________________________________________
- Date of interview: __________________________________________________
- Name of Interviewer: __________________________________________________
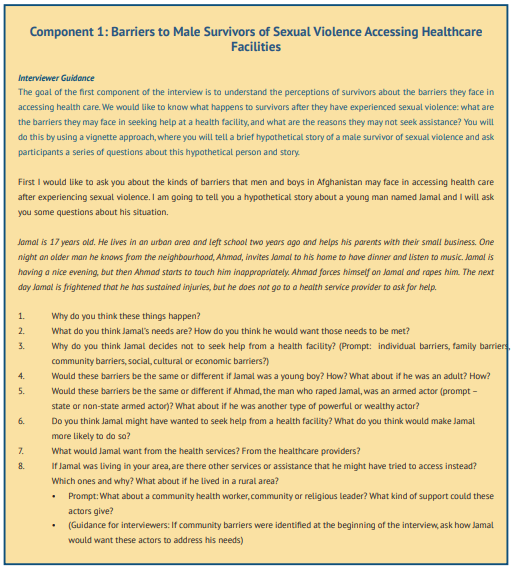
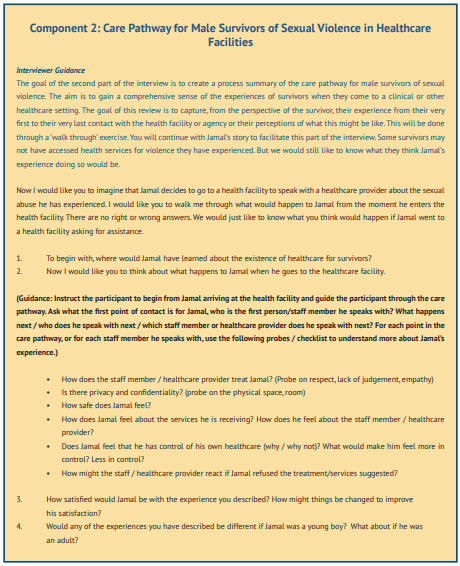

Key Informant Interviews with Healthcare Providers
Consent Form for Healthcare Staff
Hello. My name is __________ and I am working with the All Survivors Project (ASP) and Youth Health and Development Organization (YHDO). We are conducting interviews to collect information on the experiences and perspectives of healthcare providers in relation to addressing the needs of survivors of sexual violence. Women, men, girls and boys can experience sexual violence and we would like to know about your perspectives and experiences as health staff delivering services to male survivors of sexual violence. Even if you have not cared for male survivors of violence in your practice, your responses will be very helpful to us.
It is important that you know that this interview is not a measurement or appraisal of your performance. The findings from this interview will be used to understand the readiness and requirements of the health sector to strengthen healthcare response to sexual violence against men and boys. There are no direct benefits to you by participating in this interview, although your help in responding to these questions will be used to help healthcare providers deliver better services to male survivors of violence.
Due to the sensitivity of the topic, you might experience discomfort during the interview. If you feel uncomfortable at any time, you can pause or stop the interview. You can decide to skip any questions that you do not want to answer, and you are free to withdraw your participation at any time.
Your answers will be confidential. I would like to audio record the interview so that I capture our discussion correctly. After I have transcribed the interview, we will delete the audio recording. If you would prefer that I did not audio record the interview, then I can take notes of our discussion. Your name or the health facility where you work will not be included in any reports that we write about this study. We will analyse the data from this interview alongside the interviews of other healthcare providers. The only people who will have access to the interview transcript or notes are the people who are working on this study.
If you would like more information about this study, or if you would like to complain about this interview or any part of the research, you can contact Dr Rasheed the director of YHDO on (Tel: ———-).
The interview will take approximately 1 hour. If you have any questions, you can ask now, or at any point during our discussion or at the end of the interview. Do you have any questions about the study?
Do you consent to participate? Do you consent to have the interview audio recorded?
(Guidance – if the person does not consent to participate then politely thank them for their time and end the consent process. If the person consents to participate and have their interview recorded, proceed by beginning the audio recording and the interview. If the person consents to participate in the interview but does not want the interview audio recorded, then take notes of the discussion.)
Interview Guidelines for Healthcare Staff
- Province: ___________________________________________________
- District: __________________________________________________
- Name of Facility: __________________________________________________
- Gender of respondent: _____________________________________________
- Type of position of healthcare staff member: ___________________________
- Date of interview: ______________________________________________
- Name of Interviewer: ________________________________________
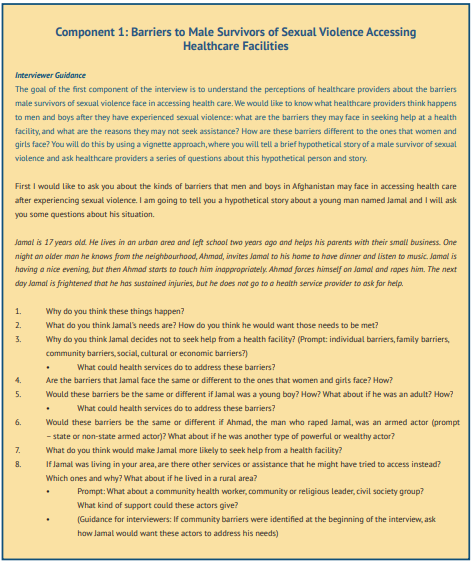
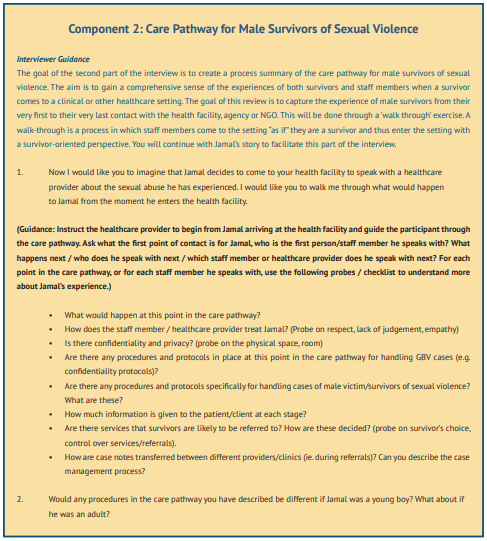
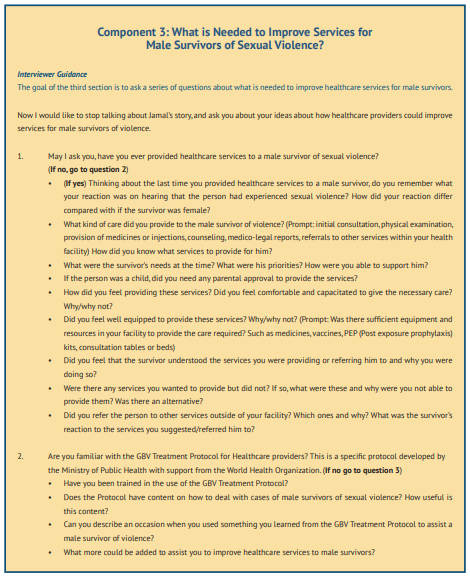
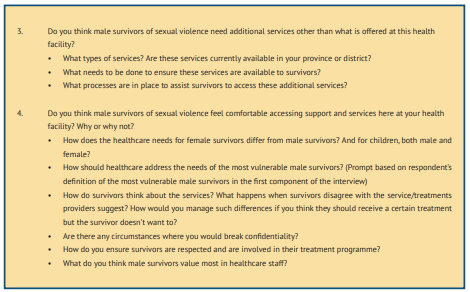
Key Informant Interviews with Community Health Workers
Consent Form for Community Health Workers
Hello. My name is __________ and I am working with the All Survivors Project (ASP) and the Youth Health and Development Organization (YHDO). We are conducting interviews to collect information on the experiences and perspectives of healthcare providers in relation to addressing the needs of survivors of sexual violence, and we are interested in including the perspectives of community health workers and mobile outreach workers since you are important actors who are in contact with and support communities and survivors. Women, men, girls and boys can experience sexual violence and we would like to know about your perspectives and experiences as community health workers supporting male survivors of sexual violence. Even if you have not cared for male survivors of sexual violence before, your responses will be very helpful to us.
It is important that you know that this interview is not a measurement or appraisal of your performance as a health worker. Community health workers are an important part of the health sector and the findings from this interview will be used to understand the readiness and requirements of the health sector to strengthen healthcare response to sexual violence against men and boys. There are no direct benefits to you by participating in this interview, although your help in responding to these questions will be used to help us understand how the health sector can deliver better services to male survivors of violence.
Due to the sensitivity of the topic, you might experience discomfort during the interview. Sometimes when people talk about difficult topics they can feel upset. If you feel uncomfortable or upset at any time, you can pause or stop the interview. If you feel that you need to speak with a counselor, please let me know as there is a counselor who I can arrange to call you and provide free and confidential counseling. We can also provide you with a list of medical or counseling services that you can access if you wish.
You can decide to skip any questions that you do not want to answer, and you are free to withdraw your participation at any time. If you do refuse to answer a question or if you decide to withdraw your participation in the interview, nobody will be upset with you and this will in no way affect your ability to access help from a counselor or from other medical or counseling service providers. Nor will it impact on your position as a community health worker.
Your answers will be confidential. I would like to audio record the interview so that I capture our discussion correctly. After I have transcribed the interview, we will delete the audio recording. If you would prefer that I did not audio record the interview, then I can take notes of our discussion. Your name or the community where you work will not be included in any reports that we write about this study. We will analyse the data from this interview alongside the interviews of other community health workers. The only people who will have access to the interview transcript or notes are the people who are working on this study.
If you would like more information about this study, or if you would like to complain about this interview or any part of the research, you can contact Dr Rasheed the director of YHDO on (Tel: ———-). If after our interview you feel upset and would like to speak with a counselor, you can also contact Dr Rasheed so that YHDO can arrange for a counselor to call you.
The interview will take approximately 1 hour. If you have any questions, you can ask now, or at any point during our discussion or at the end of the interview. Do you have any questions about the study?
Do you consent to participate? Do you consent to have the interview audio recorded?
(Guidance – if the person does not consent to participate then politely thank them for their time and end the consent process. If the person consents to participate and have their interview recorded, proceed by beginning the audio recording and the interview. If the person consents to participate in the interview but does not want the interview audio recorded, then take notes of the discussion.)
Interview Guidelines for Community Health Workers
- Province: ________________________________________
- District: ________________________________________
- Gender of respondent: ________________________________________
- Type of health worker: ( ) Community Health Worker
- Date of interview: ________________________________________
- Name of Interviewer: ________________________________________
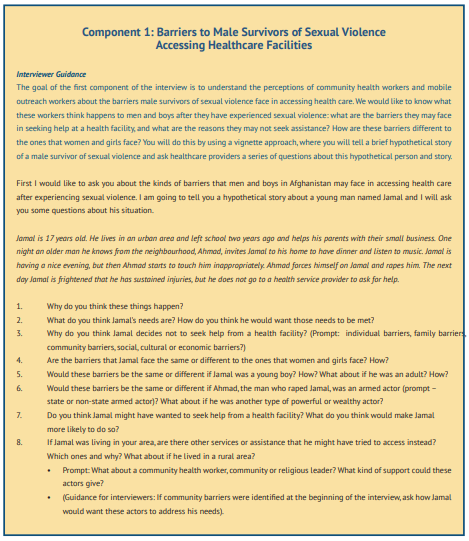
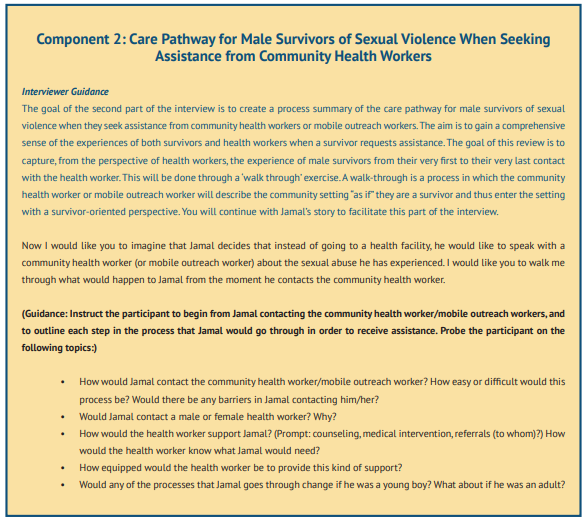
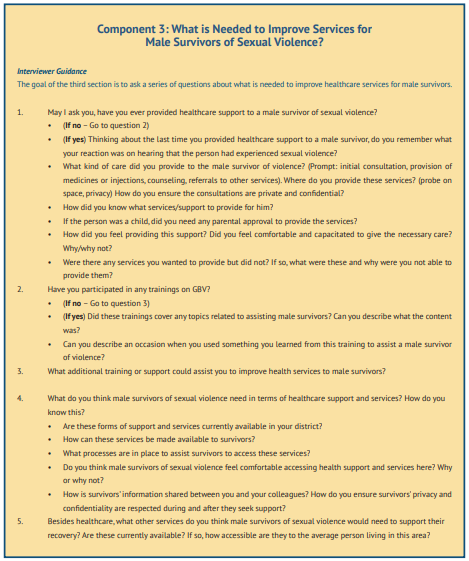
References[+]
| 1↑ | Central Statistics Organization (CSO), Ministry of Public Health (MoPH) and ICF, Afghanistan Demographic and Health Survey 2015, January 2017. |
|---|---|
| 2↑ | Afghanistan Independent Human Rights Commission, National Inquiry Report on Factors and Causes of Rape and Honor Killing in Afghanistan August 2015. |
| 3↑ | Afghanistan Independent Human Rights Commission, Summary of the Report on Violence Against Women. The Causes, Context, and Situation of Violence Against Women in Afghanistan, March 2018. |
| 4↑ | UNICEF, Children and Women in Afghanistan: A Situation Analysis 2014, November 2014. |
| 5↑ | All Survivors Project, Afghanistan, https://allsurvivorsproject.org/wp-content/uploads/2017/08/Afghanistan-2.pdf. |
| 6↑ | Islamic Republic of Afghanistan Ministry of Justice, Law on Protection of Child Rights, March 2019; See also Afghanistan Independent Human Rights Commission, Causes and Consequences of Bacha Bazi in Afghanistan (National Inquiry Report), August 2014. |
| 7↑ | Save the Children and Federal Republic of Germany Foreign Office, Learning Without Fear: A Violence-Free School Project Manual, 2011. |
| 8↑ | Save the Children, Knowledge, Attitudes and Practices on Violence and Harmful Practices Against Children in Afghanistan: A Baseline Study, August 2017. |
| 9↑ | Afghanistan Independent Human Rights Commission, Monitoring and Investigation of Alleged Child Sexual Harassment in Schools and Workplaces in Logar Province, January – February 2020. |
| 10↑ | United Nations Office on Drugs and Crime, Afghanistan: Implementing Alternatives to Imprisonment, In Line with International Standards and National Legislation. Assessment Report, May 2008. |
| 11↑ | Naz Foundation International, Rapid Assessment of Male Vulnerabilities to HIV and Sexual Exploitation in Afghanistan. Final Report, 30 March 2009. |
| 12↑ | Vu et al., ‘Integrated Behavioral and Biological Surveillance in Afghanistan: Findings of 2012 IBBS Survey and Comparison to 2009 IBBS Survey’ (unpublished), 2013, cited in Andrea Wirtz et al., ‘Uncovering the epidemic of HIV among men who have sex with men in Central Asia’, Drug and Alcohol Dependence, 132 Suppl 1: S17-24, 2013. |
| 13↑ | Islamic Republic of Afghanistan Ministry of Public Health, A Basic Package of Health Services for Afghanistan, 2009; Said Ahmad Maisam Najafizada, Ivy Lynn Bourgeault & Ronald Labonté, ‘A gender analysis of a national. |
| 14↑ | Islamic Republic of Afghanistan Ministry of Public Health, A Basic Package of Health Services for Afghanistan, 2009. |
| 15↑ | Julienne Corboz & Zulaikha Rafiq, Localisation for GBV prevention and response in Afghanistan: A Policy Study in Support of CARE’s Voices and Partnerships Against Violence (Safe from the Start) Project, CARE International UK, 2019. |
| 16↑ | Anbrasi Edward et al., ‘Toward Universal coverage in Afghanistan: A multi-stakeholder assessment of capacity investments in the community health worker system’, Social Science & Medicine, 145: 173-183, 2015. |
| 17↑ | Anne Gatuguta et al., ‘Should community health workers offer support healthcare services to survivors of sexual violence? A systematic review’, BMC International Health and Human Rights, 17: 28, 2017. |
| 18↑ | Islamic Republic of Afghanistan Ministry of Public Health, World Health Organization and United Nations Entity for Gender Equality and the Empowerment of Women (UN Women), Gender-Based Violence Treatment Protocol for Healthcare Providers in Afghanistan [hereinafter GBV Treatment Protocol], 2014. |
| 19↑ | Medica Afghanistan/medica mondiale, GBV and Trauma-Sensitive Healthcare in Afghanistan: A Baseline Study, September 2016; United Nations Population Fund, Knowledge, Attitudes and Practices Survey on Gender-Based Violence in five Provinces in Afghanistan, 2016; Dominique Day & Abdul Rasheed, Assessing the Readiness and Capacity of Health Facilities and Health Care Providers to Strengthen Health Response to Gender-Based Violence in 14 Provinces of Afghanistan, 2018. |
| 20↑ | Islamic Republic of Afghanistan Ministry of Public Health, Gender Based Violence-Psychosocial Counseling Training Packages. Module 1: Understanding Gender-Based Violence, p. 6, undated. |
| 21↑ | According to MoPH GBV data, Samangan is the province with the largest number of reported cases of sexual violence against male victims/survivors. |
| 22↑ | Sarah Chynoweth et al., ‘A social ecological approach to understanding service utilization barriers among male survivors of sexual violence in three refugee settings: a qualitative exploratory study’, Conflict and Health, 14: 43, 2020. |
| 23↑ | Hamidullah Bamik, ‘Talking about Sexual Attitudes and Behaviors: a Cultural and Social Taboo in Afghanistan’, Humanitarian and Socio-Economic Sciences Journal, 3(14), 2019. |
| 24↑ | UNFPA, Rights-based Family Life Education Helps School Children to Grow up Strong and Decisive Adults, 21 November 2017, https://bit.ly/3rPzhbc. |
| 25↑ | All Survivors Project, The Health of Male and LGBT Survivors of Conflict-Related Sexual Violence, 2020; Sarah Chynoweth et al., ‘A social ecological approach to understanding service utilization barriers among male survivors of sexual violence in three refugee settings: a qualitative exploratory study’, Conflict and Health, 14: 43, 2020; Women’s Refugee Commission, “More Than One Million Pains”: Sexual Violence Against Men and Boys on the Central Mediterranean Route to Italy, March 2019; Women’s Refugee Commission, “It’s Happening to Our Men as Well”: Sexual Violence Against Rohingya Men and Boys, November 2018. |
| 26↑ | Sarah Chynoweth et al., ‘A social ecological approach to understanding service utilization barriers among male survivors of sexual violence in three refugee settings: a qualitative exploratory study’, Conflict and Health, 14: 43, 2020. |
| 27↑ | MOSAIC (MENA Organisation for Services, Advocacy, Integration and Capacity Building), Male Survivors of Sexual Assault: A Manual on Evaluation and Management for General Practitioners, undated. |
| 28↑ | Médecin Sans Frontières, Between Rhetoric and Reality: The Ongoing Struggle to Access Healthcare in Afghanistan, February 2014. |
| 29↑ | United Nations Population Fund, Knowledge, Attitudes and Practices Survey on Gender-Based Violence in five Provinces in Afghanistan, 2016. |
| 30↑ | United Nations Population Fund, Knowledge, Attitudes and Practices Survey on Gender-Based Violence in Five Provinces in Afghanistan, 2016; Dominique Day & Abdul Rasheed, Assessing the Readiness and Capacity of Health Facilities and Health Care Providers to Strengthen Health Response to Gender-Based Violence in 14 Provinces of Afghanistan, 2018. |
| 31↑ | Sarah Chynoweth et al., ‘A social ecological approach to understanding service utilization barriers among male victim/survivors of sexual violence in three refugee settings: a qualitative exploratory study’, Conflict and Health, 14: 43, 2020. |
| 32↑ | World Health Organization and Youth Health and Development Organization, Assessment on the Capacity of Health Facilities and Health Care Providers to Respond to Gender-Based Violence in Afghanistan. Baseline Assessment, 2015. For additional information, see WHO project improves health care sector’s response to gender-based violence in Afghanistan, 18 March 2018, http://bit.ly/3lgIFly. |
| 33↑ | Dominique Day & Abdul Rasheed, Assessing the Readiness and Capacity of Health Facilities and Health Care Providers to Strengthen Health Response to Gender-Based Violence in 14 Provinces of Afghanistan, 2018. |
| 34↑ | MOSAIC, Male Survivors of Sexual Assault: A Manual on Evaluation and Management for General Practitioners, undated. |
| 35↑ | GBV Treatment Protocol, 2014. |
| 36↑ | Afghanistan Analysts Network, Widespread Violence Yet Perpetrators Go Unpunished: A new UN report on violence against Afghan women, 29 May 2018 (updated 9 March 2020); Afghanistan Public Policy Research Organization, New Penal Code and EVAW Law: To Incorporate or Not to Incorporate? July 2018. |
| 37↑ | Sayed Jalal Shajjan, The Revised Criminal Code: an End for Bacha Bazi? 24 January 2018. http://bit.ly/38DUYDG. |
| 38↑ | Islamic Republic of Afghanistan Ministry of Justice, Law on Protection of Child Rights, March 2019, p. 54. |
| 39↑ | Islamic Republic of Afghanistan Ministry of Justice, Law on Protection of Child Rights, March 2019, p. 56. |
| 40↑ | United Nations Security Council, Report of the Secretary General on Children and armed conflict in Afghanistan, UN Doc. S/2019/727, 10 September 2019. |
| 41↑ | Sexual Rights Initiative, National Sexual Rights Law and Policy Database, https://sexualrightsdatabase.org/countries/399/Afghanistan. |
| 42↑ | Islamic Republic of Afghanistan Ministry of Justice, Justice Sector Support Program translation of the final version of the Penal Code, September 2017, p. 223. |
| 43↑ | Islamic Republic of Afghanistan Ministry of Justice, Justice Sector Support Program Translation of the Final Version of the Penal Code, September 2017, p. 225 and p. 226. |
| 44↑ | Terre des Hommes, An Assessment of Juvenile Justice in Afghanistan, January 2010; United Nations Office on Drugs and Crime, Afghanistan: Implementing Alternatives to Imprisonment, in line with International Standards and National Legislation. Assessment Report, 2008. |
| 45↑ | As noted in the following section of this report on survivor-centred care (special considerations for children), sending children to forensic medical services is not necessarily in the best interests of the child, nor is obtaining parental consent to do so, particularly if the child might be placed at further risk of violence. |
| 46↑ | World Health Organization, Responding to Children and Adolescents Who Have Been Sexually Abused: WHO Clinical Guidelines, 2017. |
| 47↑ | This exercise has been adapted from a ‘Creating Cultures of Trauma-Informed Care’ (CCTIC) health care staff focus group tool that maps care pathways in health facilities. |
| 48↑ | FPCs are staffed by three service providers, including a medical doctor, a psychosocial counselor and a legal advisor. |